Abstract
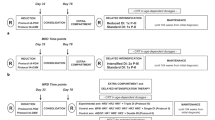
Minimal residual disease (MRD) based risk stratification criteria for specific genetic subtypes remained unclear in childhood acute lymphoblastic leukemia (ALL). Among 723 children with newly diagnosed ALL treated with the Chinese Children Leukemia Group CCLG-2008 protocol, MRD was assessed at time point 1 (TP1, at the end of induction) and TP2 (before consolidation treatment) and the MRD levels significantly differed in patients with different fusion genes or immunophenotypes (P all < 0.001). Moreover, the prognostic impact of MRD varied by distinct molecular subtypes. We stratified patients in each molecular subtype into two MRD groups based on the results. For patients carrying BCR::ABL1 or KMT2A rearrangements, we classified patients with MRD < 10–2 at both TP1 and TP2 as the low MRD group and the others as the high MRD group. ETV6::RUNX1+ patients with TP1 MRD < 10–3 and TP2 MRD-negative were classified as the low MRD group and the others as the high MRD group. For T-ALL, We defined children with TP1 MRD ≥ 10–3 as the high MRD group and the others as the low MRD group. The 10-year relapse-free survival of low MRD group was significantly better than that of high MRD group. We verified the prognostic impact of the subtype-specific MRD-based stratification in patients treated with the BCH-ALL2003 protocol. In conclusion, the subtype-specific MRD risk stratification may contribute to the precise treatment of childhood ALL.


Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Malard F, Mohty M (2020) Acute lymphoblastic leukaemia. Lancet 395(10230):1146–1162
Hunger SP, Mullighan CG (2015) Acute lymphoblastic leukemia in children. N Engl J Med 373(16):1541–1552
Bhojwani D, Pui CH (2013) Relapsed childhood acute lymphoblastic leukaemia. Lancet Oncol 14(6):e205–e217
Jia MZ et al (2023) Tracing back of relapse clones by Ig/TCR gene rearrangements reveals complex patterns of recurrence in pediatric acute lymphoblastic leukemia. Int J Lab Hematol 45(5):717–725
Zhao XS et al (2012) Monitoring MRD with flow cytometry: an effective method to predict relapse for ALL patients after allogeneic hematopoietic stem cell transplantation. Ann Hematol 91(2):183–192
Ravandi F et al (2016) Minimal residual disease assessed by multi-parameter flow cytometry is highly prognostic in adult patients with acute lymphoblastic leukaemia. Br J Haematol 172(3):392–400
O’Connor D et al (2018) Genotype-specific minimal residual disease interpretation improves stratification in pediatric acute lymphoblastic leukemia. J Clin Oncol 36(1):34–43
Pui CH et al (2017) Clinical impact of minimal residual disease in children with different subtypes of acute lymphoblastic leukemia treated with response-adapted therapy. Leukemia 31(2):333–339
Gao C et al (2012) Clinical features, early treatment responses, and outcomes of pediatric acute lymphoblastic leukemia in China with or without specific fusion transcripts: a single institutional study of 1,004 patients. Am J Hematol 87(11):1022–1027
Cui L et al (2018) Outcome of children with newly diagnosed acute lymphoblastic leukemia treated with CCLG-ALL 2008: the first nation-wide prospective multicenter study in China. Am J Hematol 93(7):913–920
Cui L et al (2010) Combined analysis of minimal residual disease at two time points and its value for risk stratification in childhood B-lineage acute lymphoblastic leukemia. Leuk Res 34(10):1314–1319
van der Velden VH et al (2007) Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 21(4):604–611
Vidriales MB et al (2003) Minimal residual disease monitoring by flow cytometry. Best Pract Res Clin Haematol 16(4):599–612
Tran TH et al (2022) Whole-transcriptome analysis in acute lymphoblastic leukemia: a report from the DFCI ALL Consortium Protocol 16–001. Blood Adv 6(4):1329–1341
Tran TH, Hunger SP (2022) The genomic landscape of pediatric acute lymphoblastic leukemia and precision medicine opportunities. Semin Cancer Biol 84:144–152
Li JF et al (2018) Transcriptional landscape of B cell precursor acute lymphoblastic leukemia based on an international study of 1,223 cases. Proc Natl Acad Sci U S A 115(50):E11711-e11720
Cui L et al (2021) Combined analysis of IKZF1 deletions and CRLF2 expression on prognostic impact in pediatric B-cell precursor acute lymphoblastic leukemia. Leuk Lymphoma 62(2):410–418
Druker BJ (2002) Perspectives on the development of a molecularly targeted agent. Cancer Cell 1(1):31–36
Schrappe M et al (2011) Late MRD response determines relapse risk overall and in subsets of childhood T-cell ALL: results of the AIEOP-BFM-ALL 2000 study. Blood 118(8):2077–2084
Faham M et al (2012) Deep-sequencing approach for minimal residual disease detection in acute lymphoblastic leukemia. Blood 120(26):5173–5180
Sala Torra O et al (2017) Next-generation sequencing in adult B cell acute lymphoblastic leukemia patients. Biol Blood Marrow Transplant 23(4):691–696
Funding
This work was supported by the National Natural Science Foundation of China, No. 81970135, No. 81870114, the Beijing Natural Science Foundation of China, No. 7202044, the New Sunshine Charity Foundation, China, No. 2017002, Funding for Reform and Development of Beijing Municipal Health Commission.
Author information
Authors and Affiliations
Contributions
HXT analyzed the data and wrote the original draft. WCJ and ZZJ collected the clinical data. GC and XTL performed the experiments. WTY, WMY and ZRD made clinical contributions. LZG , CL and ZRD designed the research and revised the paper. All authors were involved in the final approval of the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, XT., Wang, CJ., Gao, C. et al. Relationship between subtype-specific minimal residual disease level and long-term prognosis in children with acute lymphoblastic leukemia. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05687-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05687-y