Abstract
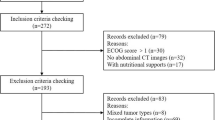
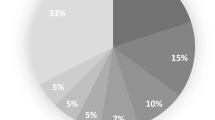
Cancer cachexia is a disorder that affects patient outcomes. The present study prospectively evaluated the prognostic value of the cachexia index (CXI) in elderly patients with non-Hodgkin’s lymphoma (NHL). We prospectively analyzed 51 elderly patients who were diagnosed with NHL at our institution. CXI was calculated as follows: CXI = SMI × Alb/NLR (SMI: skeletal muscle index, Alb: serum albumin, NLR: neutrophil-to-lymphocyte ratio). SMI was measured by a bioelectrical impedance analysis (BIA) using the InBody 720. We determined the sex-specific cutoff values of the CXI by a receiver operating characteristic curve analysis and divided all patients into low- and high-CXI groups. The median age at the diagnosis was 78 years (60–93 years), and 28 (55%) were male. The histologic subtypes were B-cell lymphoma in 49 patients and T-cell lymphoma in 2. Twenty-eight (55%) patients were categorized into the high-CXI group, and 23 (45%) were categorized into the low-CXI group. The overall survival (OS) in the low-CXI group was significantly shorter than that in the high-CXI group (3-year OS, 70.4% vs. 95.7%, p = 0.007). Among 23 patients with DLBCL, patients with low-CXI had shorter OS than those with high-CXI (3-year OS, 55.6% vs. 92.9%, p = 0.008). On the other hand, sarcopenia had less impact on the clinical outcome of DLBCL patients. Low-CXI was associated with poor outcomes in elderly NHL and the CXI may be a clinical useful index for predicting prognosis. Further large prospective studies are needed to verify this conclusion.


Similar content being viewed by others
Data availability
The data sets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Vaughan VC, Mattin P, Lewandowski PA (2013) Cancer cachexia: Impact, mechanism and emerging treatments. J Cachexia Sarcopenia Muscle 4:95–109
Fearon KC, Glass DJ, Guttridge DC. Cancer cachexia: Mediators, signaling, and metabolic pathways Cell Metab 16:153–166
Loumaye A, Thissen JP (2017) Biomarkers of cancer cachexia. Clin Biochem 50(18):1281–1288
Poisson J, Martinez-Tapia C, Heitz D et al (2021) Prevalence and prognostic impact of cachexia among older patients with cancer: a nationwide cross-sectional survey (NutriAgeCancer). J Cachexia Sarcopenia Muscle 12(6):1477–1488
Schmidt SF, Rohm M, Herzig S, Diaz MB (2018) Cancer cachexia: More than skeletal muscle wasting. Trends Cancer 4(12):849–860
Go SI, Park MJ, Lee GW (2021) Clinical significance of the cachexia index in patients with small cell lung cancer. BMC Cancer 21(1):563–571
Goh MJ, Kang W, Jeong WK et al (2022) Prognostic significance of cachexia index in patients with advanced hepatocellular carcinoma treated with systemic chemotherapy. Sci Rep 12(1):7647
Go SI, Park MJ, Park S et al (2021) Cachexia index as a potential biomarker for cancer cachexia and a prognostic indicator in diffuse large B-cell lymphoma. J Cachexia Sarcopenia Muscle 12(6):2211–2219
Karmali R, Alrifai T, Fughhi IAM et al (2017) Impact of cachexia on outcomes in aggressive lymphomas. Ann Hematol 96(6):951–956
Jafri S, Previgliano C, Khandelwal K, Shi R (2015) Cachexia index in advanced non-small-cell lung cancer patients. Clin Med Insights Oncol 9:87–93
Bahat G, Turkmen BO, Aliyev S et al (2021) Cut-off values of skeletal muscle index and psoas muscle index L3 vertebra level by computerized tomography to assess low muscle mass. Clin Nutr 40(6):4360–4365
Zwart AT, Becker JN, Lamers MJ et al (2021) Skeletal muscle mass and sarcopenia can be determined with 1.5-T and 3-T neck MRI scans, in the event that no neck CT scan is performed. Eur Radiol 31(6):4053–4062
Walowski CO, Braun W, Maisch MJ et al (2020) Reference values for skeletal muscle mass – Current concepts and methodological considerations. Nutrients 12(3):755
Cheng KY, Chow SK, Hung VW et al (2021) Diagnosis of sarcopenia by evaluating skeletal muscle mass by adjusted bioimpedance analysis validated with dual-energy X-ray absorptiometry. J Cachexia Sarcopenia Muscle 12(6):2163–2173
Aleixo GFP, Shachar SS, Nyrop KA, Muss HB, Battaglini CL, Williams GR (2020) Bioelectrical impedance analysis for the assessment of sarcopenia in patients with cancer: a systematic review. Oncologist 25:170–182
Ida S, Watanabe M, Yoshida N et al (2015) Sarcopenia is a Predictor of Postoperative Respiratory Complications in Patients with Esophageal Cancer. Ann Surg Oncol 22(13):4432–4437
Wang F, Zhen HN, Wang HP, Yu K (2023) Measurement of sarcopenia in lung cancer inpatients and its association with frailty, nutritional risk, and malnutrition. Front Nutr 17(10):1143213
Chen LK, Woo J, Assantachai P et al (2020) Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 21:300–307
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458
Yamada M, Nishiguchi S, Fukutani N et al (2013) Prevalence of sarcopenia in community-dwelling Japanese older adults. JAMDA 14(12):911–915
Pierik V, Meskers C, Ancum J et al (2017) High risk of malnutrition is associated with low muscle mass in older hospitalized patients – a prospective cohort study. BMC Geriatr 17:118
Kim D, Sun J, Lee Y et al (2019) Comparative assessment of skeletal muscle mass using computerized tomography and bioelectrical impedance analysis in critically ill patients. Clin Nutr 38(6):2747–2755
Fukuda Y, Yamamoto K, Hirao M et al (2016) Sarcopenia is associated with severe postoperative complications in elderly gastric cancer patients undergoing gastrectomy. Gastric Cancer 19(3):986–993
Hara N, Iwasa M, Sugimoto R et al (2016) Sarcopenia and sarcopenic obesity are prognostic factors for overall survival in patients with cirrhosis. Intern Med 55(8):863–870
Nishikawa H, Goto M, Fukunishi S, Asai A, Nishiguchi S, Higuchi K (2021) Cancer cachexia: its mechanism and clinical significance. Int J Mol Sci 22(16):8491
Fearon K, Strasser F, Anker SD et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12(5):489–495
Sadeghi M, Keshavarz-Fathi M, Baracos V et al (2018) Cancer cachexia: Diagnosis, assessment, and treatment. Crit Rev Oncol Hematol 127:91–104
Xu XT, He DL, Tian MX, Wu HJ, Jin X (2022) Prognostic value of sarcopenia in patients with diffuse large B-cell lymphoma treated with R-CHOP: A systematic review and meta-analysis. Front Nutr 9:816883
Camus V, Lanic H, Kraut J et al (2014) Prognostic impact of fat tissue loss and cachexia assessed by computed tomography scan in elderly patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Eur J Haematol 93(1):9–18
Wei X, Zheng J, Zhang Z et al (2021) Consecutive hypoalbuminemia predicts inferior outcome in patients with diffuse large b-cell lymphoma. Front Oncol 10:610681
Wang J, Zhou X, Liu Y et al (2017) Prognostic significance of neutrophil-to-lymphocyte ratio in diffuse large B-cell lymphoma: A meta-analysis. PLoS One 12(4):e0176008
Funding
No specific funding was obtained to support the conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from the patients. The study was approved by the Ethics Committee of Yokohama Municipal Citizen’s Hospital.
Conflict of interest
All authors have no potential conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okubo, S., Shinmura, K., Kadota, S. et al. Evaluation of the cachexia index using a bioelectrical impedance analysis in elderly patients with non-Hodgkin’s lymphoma: A single-center prospective study. Ann Hematol 103, 823–831 (2024). https://doi.org/10.1007/s00277-023-05548-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05548-0