Abstract
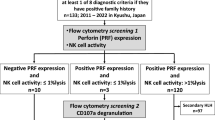
To analyze the genetic variation and prognosis of primary hemophagocytic lymphohistiocytosis (pHLH) in children and the clinical features of isolated central nervous system HLH (CNS-HLH). We retrospectively analyzed the clinical and genetic data of 480 HLH children admitted to our hospital from September 2017 to September 2022. There were 66 patients (13.75%) with pHLH, and the median age was 3.21 years (0.17–12.92 years). Variants in UNC13D (22/66, 33.33%), PRF1 (20/66, 30.30%) and XIAP (11/66, 16.67%) were the most common. More CNS involvement was observed in pHLH patients than in secondary hemophagocytic lymphohistiocytosis (sHLH) patients (50% vs. 25.3%, P = 0.001). Eight pHLH patients had isolated CNS-HLH at onset, which progressed to systemic HLH within 10–30 days to several years. Among them, five patients who underwent hematopoietic stem cell transplantation (HSCT) survived without CNS sequelae, and the three patients who did not undergo HSCT died of disease progression or recurrence. Determination of natural killer (NK) cell cytotoxicity and CD107a levels had low sensitivity and specificity in the diagnosis of pHLH, especially in patients with PRF1 and XIAP mutations. The 3-year overall survival (OS) was significantly lower in pHLH patients than in sHLH patients (74.5% ± 14.7% vs. 89.2% ± 3.53%, P = 0.021) and in patients with CNS involvement than in those without (53.8% ± 26.07% vs. 94.4% ± 10.58%, P = 0.012). There was a significant difference in OS among pHLH patients with different gene variants (P = 0.032); patients with PRF1 variants had poor 3-year OS, and patients with XIAP variants had good 3-year OS (50% ± 28.22% and 100%, respectively). pHLH patients with distinct variants have different prognoses. Isolated CNS-HLH patients are easily misdiagnosed, and HSCT may be beneficial for these patients. Determination of NK cell cytotoxicity and CD107a levels cannot precisely distinguish pHLH from sHLH.



Similar content being viewed by others
References
Fujiwara F, Hibi S, Imashuku S (1993) Hypercytokinemia in hemophagocytic syndrome. Am J Pediatr Hematol Oncol 15(1):92–98
Henter JI, Elinder G, Söder O et al (1991) Hypercytokinemia in familial hemophagocytic lymphohistiocytosis. Blood 78(11):2918–2922
Ramos-Casals M, Brito-Zerón P, López-Guillermo A et al (2014) Adult haemophagocytic syndrome. Lancet 383(9927):1503–1516
Yao S, Wang Y, Sun Y et al (2021) Epidemiological investigation of hemophagocytic lymphohistiocytosis in China. Orphanet J Rare Dis 16(1):342
Canna SW, Marsh RA (2020) Pediatric hemophagocytic lymphohistiocytosis. Blood 135(16):1332–1343
Bousfiha A, Moundir A, Tangye SG et al (2022) The 2022 update of IUIS phenotypical classification for human inborn errors of immunity. J Clin Immunol 42(7):1508–1520
Brisse E, Matthys P, Wouters CH (2016) Understanding the spectrum of haemophagocytic lymphohistiocytosis: update on diagnostic challenges and therapeutic options. Br J Haematol 174(2):175–187
Blincoe A, Heeg M, Campbell PK et al (2020) Neuroinflammatory disease as an isolated manifestation of hemophagocytic lymphohistiocytosis. J Clin Immunol 40(6):901–916
Bucciol G, Willemyns N, Verhaaren B et al (2022) Child neurology: familial hemophagocytic lymphohistiocytosis underlying isolated central nervous system inflammation. Neurology 99:660–664
Henter JI, Horne A, Aricó M et al (2007) HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 48(2):124–131
Taieb G, Kaphan E, Duflos C et al (2021) Hemophagocytic lymphohistiocytosis gene mutations in adult patients presenting with CLIPPERS-Like syndrome. Neurol Neuroimmunol Neuroinflamm 8(3):e970
Zhang J, Sun Y, Shi X et al (2020) Genotype characteristics and immunological indicator evaluation of 311 hemophagocytic lymphohistiocytosis cases in China. Orphanet J Rare Dis 15(1):112
Madkaikar MR, Shabrish S, Kulkarni M et al (2019) Application of flow cytometry in primary immunodeficiencies: experience from India. Front Immunol 10:1248
Marcenaro S, Gallo F, Martini S et al (2006) Analysis of natural killer-cell function in familial hemophagocytic lymphohistiocytosis (FHL): defective CD107a surface expression heralds Munc13-4 defect and discriminates between genetic subtypes of the disease. Blood 108(7):2316–2323
Abdalgani M, Filipovich AH, Choo S et al (2015) Accuracy of flow cytometric perforin screening for detecting patients with FHL due to PRF1 mutations. Blood 126(15):1858–1860
Johnson TS, Villanueva J, Filipovich AH et al (2011) Contemporary diagnostic methods for hemophagocytic lymphohistiocytic disorders. J Immunol Methods 364(1–2):1–13
Marsh RA, Jordan MB, Filipovich AH (2011) Reduced-intensity conditioning haematopoietic cell transplantation for haemophagocytic lymphohistiocytosis: an important step forward. Br J Haematol 154(5):556–563
Mo W, Wei W, Sun Y et al (2019) Application of blood and immunodeficiency gene detection in the diagnosis of hemophagocytic lymphohistiocytosis patients. Exp Hematol 78:62–69
Chen X, Wang F, Zhang Y et al (2018) Genetic variant spectrum in 265 Chinese patients with hemophagocytic lymphohistiocytosis: Molecular analyses of PRF1, UNC13D, STX11, STXBP2, SH2D1A, and XIAP. Clin Genet 94(2):200–212
Gadoury-Levesque V, Dong L, Su R et al (2020) Frequency and spectrum of disease-causing variants in 1892 patients with suspected genetic HLH disorders. Blood Adv 4(12):2578–2594
Meeths M, Chiang SC, Wood SM et al (2011) Familial hemophagocytic lymphohistiocytosis type 3 (FHL3) caused by deep intronic mutation and inversion in UNC13D. Blood 118(22):5783–5793
Bąbol-Pokora K, Wołowiec M, Popko K et al (2021) Molecular genetics diversity of primary hemophagocytic lymphohistiocytosis among polish pediatric patients. Arch Immunol Ther Exp (Warsz) 69(1):31
Gao Z, Wang Y, Wang J et al (2019) Soluble ST2 and CD163 as potential biomarkers to differentiate primary hemophagocytic lymphohistiocytosis from macrophage activation syndrome. Mediterr J Hematol Infect Dis 11(1):e2019008
Benallegue N, Beaudonnet F, Husson B et al (2021) Neurological involvement in secondary hemophagocytic lymphohistiocytosis in children. Eur J Paediatr Neurol 34:110–117
Horne A, Trottestam H, Aricò M et al (2008) Frequency and spectrum of central nervous system involvement in 193 children with haemophagocytic lymphohistiocytosis. Br J Haematol 140(3):327–335
Locatelli F, Jordan MB, Allen C et al (2020) Emapalumab in children with primary hemophagocytic lymphohistiocytosis. N Engl J Med 382(19):1811–1822
Ma W, Li XJ, Li W et al (2021) MRI findings of central nervous system involvement in children with haemophagocytic lymphohistiocytosis: correlation with clinical biochemical tests. Clin Radiol 76(2):159.e159-159.e117
Benson LA, Li H, Henderson LA et al (2019) Pediatric CNS-isolated hemophagocytic lymphohistiocytosis. Neurol Neuroimmunol Neuroinflamm 6(3):e560
Wegehaupt O, Wustrau K, Lehmberg K et al (2020) Cell versus cytokine - directed therapies for hemophagocytic lymphohistiocytosis (HLH) in inborn errors of immunity. Front Immunol 11:808
Rubin TS, Zhang K, Gifford C et al (2017) Perforin and CD107a testing is superior to NK cell function testing for screening patients for genetic HLH. Blood 129(22):2993–2999
Hines MR, Nichols KE (2017) Go with the flow: perforin and CD107a in HLH. Blood 129(22):2954–2955
Bryceson YT, Pende D, Maul-Pavicic A et al (2012) A prospective evaluation of degranulation assays in the rapid diagnosis of familial hemophagocytic syndromes. Blood 119(12):2754–2763
Acknowledgements
The authors would like to thank: Beijing Municipal Science & Technology Commission (No. Z221100007422054), the Special Fund of the Pediatric Medical Coordinated Development Center of Beijing Municipal Administration (No. XTZD20180202), Beijing research ward project (No. BCRW202101), Funding for Reform and development of Beijing Municipal Health Commission.
Funding
This work was supported by Beijing Municipal Science & Technology Commission (No. Z221100007422054), the Special Fund of the Pediatric Medical Coordinated Development Center of Beijing Municipal Administration (No. XTZD20180202), Beijing research ward project (No. BCRW202101), Funding for Reform and development of Beijing Municipal Health Commission.
Author information
Authors and Affiliations
Contributions
Zhigang Li: Funding acquisition, Supervision, Data curation, Writing-Reviewing and Editing. Chenzi Zhao: Conceptualization, Methodology, Investigation, oversight, Data curation, Writing-Original draft preparation. Qing Zhang: Conceptualization, Methodology, Investigation, oversight, Data curation. Hongyun Lian: Data curation. Honghao Ma: Data curation. Xiaoxi Zhao: Data curation. Rui Zhang: Data curation.
Corresponding author
Ethics declarations
Financial interests
The authors declare they have no financial interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board (IRB) of Beijing Children’s Hospital, Capital Medical University (Number:2018-71).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, C., Zhang, Q., Zhang, R. et al. Genetic and clinical characteristics of primary hemophagocytic lymphohistiocytosis in children. Ann Hematol 103, 17–28 (2024). https://doi.org/10.1007/s00277-023-05499-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05499-6