Abstract
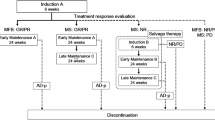
Rosai Dorfman disease (RDD) is a non-Langerhans cell histiocytic neoplasm characterized by sinus histiocytosis with variable emperipolesis. There is a limited understanding of the factors that contribute to disease progression. Traditional management of RDD consists of local therapies (resection, radiation) for localized disease and myelosuppression for systemic disease; targeted medications have also recently been introduced into clinical practice as an additional therapeutic modality. The goals of this study are to compare the impact of targeted therapies to conventional management of RDD and identify trends in laboratory data that may provide insight into disease progression. A retrospective analysis was conducted at a single institution over a 20-year period in 35 adult patients with histopathologic evidence of RDD without confounding secondary malignancies. Clinical data points included laboratory evaluation, molecular diagnostics, imaging, and therapies rendered. Binary data was utilized for statistical analysis and comparison of outcomes by treatment type and utilization of targeted agents. Evaluation of treatment response varied based on anatomic disease sites and baseline imaging modality. To standardize the radiographic analysis, we included PERCIST (if PET was utilized) or RECIST assessments (in the cases of CT or MR imaging). Conventional therapies rendered included local treatment (surgery, radiation, intralesional injections), systemic corticosteroids, immunotherapy, and chemotherapy while targeted agents included only small molecule inhibitors. In this analysis, primary disease was identified in cutaneous, osseous, and CNS structures (17, 11, and 6/35 patients respectively). Management consisted of surgery (12/35 patients), steroid and myelosuppressive therapies (9/35 each), immunotherapy (5/35), and targeted molecular agents (5/35). In evaluating outcomes, the proportion of partial responses was substantially higher in recipients of molecular as compared to conventional therapy (4/5 patients compared to 6/29) while complete responses were more common in the conventional therapy cohort (12/29 compared to 1/5). Lastly, an evaluation of peripheral blood absolute monocytes in all patients who had progressed on therapy identified a significant decrease in pre-progression values as compared to values following therapy re-institution (averages of 0.70 and 0.27 K/µL, respectively; p = 0.0002, 95% CI 0.652–0.2360). Larger-scale studies are needed to further evaluate the relevance of the monocyte trends that were identified in terms of their relationship to disease status. This study is the largest analysis of Rosai Dorfman disease, that we are aware of, from a single institution. In this cohort, the utilization of small molecule inhibitors corresponded to a greater increase in partial responses than conventional therapies, although the opposite effect has been observed in complete responses. This finding can be attributed to the recent introduction of targeted agents and shorter follow-up. We anticipate higher complete response rates with the use of small molecule in ongoing analyses over a longer follow-up period. The recognition of relative monocyte elevation prior to disease progression is an intriguing and to our knowledge, novel finding in the field of Rosai Dorfman disease. Future studies aimed at elucidating the implications of this trend are in progress.





Similar content being viewed by others
References
Abla O, Jacobsen E, Picarsic J, Krenova Z, Jaffe R, Emile JF et al (2018) Consensus recommendations for the diagnosis and clinical management of Rosai-Dorfman-Destombes disease. Blood 131(26):2877–2890
Salama HA, Jazieh AR, Alhejazi AY, Absi A, Alshieban S, Alzahrani M et al (2021) Highlights of the Management of adult histiocytic disorders: Langerhans cell histiocytosis, Erdheim-Chester disease, Rosai-Dorfman disease, and hemophagocytic lymphohistiocytosis. Clin Lymphoma Myeloma Leuk 21(1):e66–e75
Aaroe A, Kurzrock R, Goyal G, Goodman AM, Patel H, Ruan G et al (2023) Successful treatment of non-Langerhans cell histiocytosis with the MEK inhibitor trametinib: a multicenter analysis. Blood Adv 7(15):3984–3992
Costelloe CM, Chuang HH, Madewell JE, Ueno NT (2010) Cancer response criteria and bone metastases: RECIST 1.1, MDA and PERCIST. J Cancer 1:80–92
Abeykoon JP, Rech KL, Young JR, Ravindran A, Ruan GJ, Dasari S et al (2022) Outcomes after treatment with cobimetinib in patients with Rosai-Dorfman disease based on KRAS and MEK alteration status. JAMA Oncol 8(12):1816–1820
Dong RF, Gong LH, Zhang W, Li L, Sun XQ, Zhang M et al (2020) Primary intraosseous Rosai-Dorfman disease: a clinicopathological analysis of fourteen cases. Zhonghua Bing Li Xue Za Zhi 49(9):904–909
Weng X, Yang Y, Zhang M, Cai C, Sun Y, Wu X et al (2022) Primary intraosseous Rosai-Dorfman disease: an analysis of clinicopathologic characteristics, molecular genetics, and prognostic features. Front Oncol 12:950114
Sandoval-Sus JD, Sandoval-Leon AC, Chapman JR, Velazquez-Vega J, Borja MJ, Rosenberg S et al (2014) Rosai-Dorfman disease of the central nervous system: report of 6 cases and review of the literature. Med Balt 93(3):165–175
Olingy CE, Dinh HQ, Hedrick CC (2019) Monocyte heterogeneity and functions in cancer. J Leukoc Biol 106(2):309–322
Tzankov A, Kremer M, Leguit R, Orazi A, van der Walt J, Gianelli U et al (2018) Histiocytic cell neoplasms involving the bone marrow: summary of the workshop cases submitted to the 18th Meeting of the European Association for Haematopathology (EAHP) organized by the European Bone Marrow Working Group, Basel 2016. Ann Hematol 97(11):2117–2128
Jongsma MLM, Neefjes J, Spaapen RM (2021) Playing hide and seek: tumor cells in control of MHC class I antigen presentation. Mol Immunol 136:36–44
Papo M, Cohen-Aubart F, Trefond L, Bauvois A, Amoura Z, Emile JF et al (2019) Systemic histiocytosis (Langerhans cell histiocytosis, Erdheim-Chester disease, Destombes-Rosai-Dorfman disease): from oncogenic mutations to inflammatory disorders. Curr Oncol Rep 21(7):62
Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES (2011) The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood. 117(19):5019–32
Garces S, Medeiros LJ, Patel KP, Li S, Pina-Oviedo S, Li J et al (2017) Mutually exclusive recurrent KRAS and MAP2K1 mutations in Rosai-Dorfman disease. Mod Pathol 30(10):1367–1377
Janku F, Diamond EL, Goodman AM, Raghavan VK, Barnes TG, Kato S et al (2019) Molecular profiling of tumor tissue and plasma cell-free DNA from patients with non-Langerhans cell histiocytosis. Mol Cancer Ther 18(6):1149–1157
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This research did involve human participants and was performed under the University of Michigan Institutional Review Board (IRB) study ID HUM00214315. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Data Availability
Not applicable for this publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reynolds, S.B., Wilcox, S., Li, Q. et al. Investigating the correlation between small molecular inhibitor utilization, peripheral blood monocytes, and treatment outcomes in Rosai Dorfman disease. Ann Hematol 103, 37–59 (2024). https://doi.org/10.1007/s00277-023-05494-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05494-x