Abstract
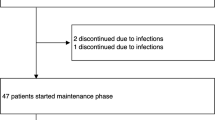
Data on mTOR inhibitors (mTORi) in autoimmune cytopenia (AIC), in adults are scarce. We retrospectively analysed 30 cases of refractory or relapsing AIC treated with an mTORi-based therapy. Eleven warm autoimmune hemolytic anaemia, 10 autoimmune thrombocytopenia, 6 acquired pure red cell aplasia, 3 autoimmune neutropenia were included. Twenty were multilineage AIC (67%) and 21 were secondary AIC (70%). mTORi were associated with other therapies in 23 AIC (77%). Twenty-two AIC (73%) responded to mTORi-based therapy: 5 reached a partial response (17%) and 17 a complete response (57%). Survival without unfavourable outcome (failure, requirement of a new therapy, or death) was longer in multilineage AIC compared to single-lineage AIC (p = 0.049) with a median event-free survival of 48 versus 12 months. Median event-free survival was 48 months in secondary AIC and 33 months in primary AIC (p = 0.79). mTORi were discontinued in 4 patients (15%) for safety reasons and in 3 patients for patient’s choice (12%). In conclusion, mTORi could be considered as an alternative or an add-on therapy in refractory or relapsing AIC in adult patients, especially in multilineage AIC.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Sawada K, Fujishima N, Hirokawa M (2008) Acquired pure red cell aplasia: updated review of treatment. Br J Haematol 142:505–514. https://doi.org/10.1111/j.1365-2141.2008.07216.x
Means RT (2016) Pure red cell aplasia. Blood 128:2504–2509. https://doi.org/10.1182/blood-2016-05-717140
Rodeghiero F, Stasi R, Gernsheimer T et al (2009) Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood 113:2386–2393. https://doi.org/10.1182/blood-2008-07-162503
Provan D, Arnold DM, Bussel JB et al (2019) Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv 3:3780–3817. https://doi.org/10.1182/bloodadvances.2019000812
Jäger U, Barcellini W, Broome CM et al (2020) Diagnosis and treatment of autoimmune hemolytic anemia in adults: Recommendations from the First International Consensus Meeting. Blood Rev 41:100648. https://doi.org/10.1016/j.blre.2019.100648
Fioredda F, Dufour C, Höglund P et al (2023) Autoimmune neutropenias: update on clinical and biological features in children and adults. HemaSphere 7:e814. https://doi.org/10.1097/HS9.0000000000000814
Evans RS, Takahashi K, Duane RT et al (1951) Primary thrombocytopenic purpura and acquired hemolytic anemia; evidence for a common etiology. AMA Arch Intern Med 87:48–65. https://doi.org/10.1001/archinte.1951.03810010058005
Miano M, Guardo D, Grossi A et al (2022) Underlying inborn errors of immunity in patients with Evans syndrome and multilineage cytopenias: a single-centre analysis. Front Immunol 13:869033. https://doi.org/10.3389/fimmu.2022.869033
Kumar D, Nguyen TH, Bennett CM et al (2022) mTOR inhibition attenuates cTfh cell dysregulation and chronic T cell activation in multi-lineage immune cytopenias. Blood blood.2022015966. https://doi.org/10.1182/blood.2022015966
Barcellini W, Giannotta JA, Fattizzo B (2021) Autoimmune complications in hematologic neoplasms. Cancers 13:1532. https://doi.org/10.3390/cancers13071532
Visco C, Barcellini W, Maura F et al (2014) Autoimmune cytopenias in chronic lymphocytic leukemia. Am J Hematol 89:1055–1062. https://doi.org/10.1002/ajh.23785
Hamblin T (2006) Autoimmune complications of chronic lymphocytic leukemia. Semin Oncol 33:230–239. https://doi.org/10.1053/j.seminoncol.2006.01.011
Jung J-H, Soh M-S, Ahn Y-H et al (2016) Thrombocytopenia in systemic lupus erythematosus: clinical manifestations, treatment, and prognosis in 230 patients. Medicine (Baltimore) 95:e2818. https://doi.org/10.1097/MD.0000000000002818
Zhou J-C, Wu M-Q, Peng Z-M et al (2020) Clinical analysis of 20 patients with non-Hodgkin lymphoma and autoimmune hemolytic anemia: a retrospective study. Medicine (Baltimore) 99:e19015. https://doi.org/10.1097/MD.0000000000019015
Crickx E, Poullot E, Moulis G et al (2019) Clinical spectrum, evolution, and management of autoimmune cytopenias associated with angioimmunoblastic T-cell lymphoma. Eur J Haematol 103:35–42. https://doi.org/10.1111/ejh.13239
Fattizzo B, Michel M, Giannotta JA et al (2021) Evans syndrome in adults: an observational multicenter study. Blood Adv 5:5468–5478. https://doi.org/10.1182/bloodadvances.2021005610
Euvrard S, Morelon E, Rostaing L et al (2012) Sirolimus and secondary skin-cancer prevention in kidney transplantation. N Engl J Med 367:329–339. https://doi.org/10.1056/NEJMoa1204166
Guba M, Pratschke J, Hugo C et al (2010) Renal function, efficacy, and safety of sirolimus and mycophenolate mofetil after short-term calcineurin inhibitor-based quadruple therapy in de novo renal transplant patients: one-year analysis of a randomized multicenter trial. Transplantation 90:175–183. https://doi.org/10.1097/TP.0b013e3181e11798
Miano M, Calvillo M, Palmisani E et al (2014) Sirolimus for the treatment of multi-resistant autoimmune haemolytic anaemia in children. Br J Haematol 167:571–574. https://doi.org/10.1111/bjh.13010
Miano M, Scalzone M, Perri K et al (2015) Mycophenolate mofetil and Sirolimus as second or further line treatment in children with chronic refractory Primitive or Secondary Autoimmune Cytopenias: a single centre experience. Br J Haematol 171:247–253. https://doi.org/10.1111/bjh.13533
Bride KL, Vincent T, Smith-Whitley K et al (2016) Sirolimus is effective in relapsed/refractory autoimmune cytopenias: results of a prospective multi-institutional trial. Blood 127:17–28. https://doi.org/10.1182/blood-2015-07-657981
Jasinski S, Weinblatt ME, Glasser CL (2017) Sirolimus as an effective agent in the treatment of immune thrombocytopenia (ITP) and Evans syndrome (ES): a single institution’s experience. J Pediatr Hematol Oncol 39:420–424. https://doi.org/10.1097/MPH.0000000000000818
Miano M, Rotulo GA, Palmisani E et al (2018) Sirolimus as a rescue therapy in children with immune thrombocytopenia refractory to mycophenolate mofetil. Am J Hematol 93:E175–E177. https://doi.org/10.1002/ajh.25119
Long Z, Yu F, Du Y et al (2018) Successful treatment of refractory/relapsed acquired pure red cell aplasia with sirolimus. Ann Hematol 97:2047–2054. https://doi.org/10.1007/s00277-018-3431-5
Feng Y, Xiao Y, Yan H et al (2020) Sirolimus as rescue therapy for refractory/relapsed immune thrombocytopenia: results of a single-center, prospective single-arm study. Front Med 7:110. https://doi.org/10.3389/fmed.2020.00110
Chen Z, Liu X, Chen M et al (2020) Successful sirolimus treatment of patients with pure red cell aplasia complicated with renal insufficiency. Ann Hematol 99:737–741. https://doi.org/10.1007/s00277-020-03946-2
Li H, Ji J, Du Y et al (2020) Sirolimus is effective for primary relapsed/refractory autoimmune cytopenia: a multicenter study. Exp Hematol 89:87–95. https://doi.org/10.1016/j.exphem.2020.08.001
Wu C, Wang Q, Xu D et al (2021) Sirolimus for patients with connective tissue disease-related refractory thrombocytopenia: a single-arm, open-label clinical trial. Rheumatol Oxf Engl 60:2629–2634. https://doi.org/10.1093/rheumatology/keaa645
Xie W, Ji L, Zhang Z (2022) Sirolimus monotherapy for thrombocytopenia in primary antiphospholipid syndrome: a pilot study from a tertiary referral center. Front Immunol 13:857424. https://doi.org/10.3389/fimmu.2022.857424
Y Y, Z T, Y H et al (2023) Sirolimus versus cyclosporine A in patients with primary acquired pure red cell aplasia: a prospective cohort study. Blood Cancer J 13. https://doi.org/10.1038/s41408-023-00845-3
Malphettes M, Gérard L, Carmagnat M et al (2009) Late-onset combined immune deficiency: a subset of common variable immunodeficiency with severe T cell defect. Clin Infect Dis Off Publ Infect Dis Soc Am 49:1329–1338. https://doi.org/10.1086/606059
Oliveira JB, Bleesing JJ, Dianzani U et al (2010) Revised diagnostic criteria and classification for the autoimmune lymphoproliferative syndrome (ALPS): report from the 2009 NIH International Workshop. Blood 116:e35-40. https://doi.org/10.1182/blood-2010-04-280347
Boursiquot J-N, Gérard L, Malphettes M et al (2013) Granulomatous disease in CVID: retrospective analysis of clinical characteristics and treatment efficacy in a cohort of 59 patients. J Clin Immunol 33:84–95. https://doi.org/10.1007/s10875-012-9778-9
Egg D, Rump IC, Mitsuiki N et al (2022) Therapeutic options for CTLA-4 insufficiency. J Allergy Clin Immunol 149:736–746. https://doi.org/10.1016/j.jaci.2021.04.039
Tesch VK, Abolhassani H, Shadur B et al (2020) Long-term outcome of LRBA deficiency in 76 patients after various treatment modalities as evaluated by the immune deficiency and dysregulation activity (IDDA) score. J Allergy Clin Immunol 145:1452–1463. https://doi.org/10.1016/j.jaci.2019.12.896
Li J, Wang Z, Dai L et al (2013) Effects of rapamycin combined with low dose prednisone in patients with chronic immune thrombocytopenia. Clin Dev Immunol 2013:548085. https://doi.org/10.1155/2013/548085
Author information
Authors and Affiliations
Contributions
BS, MM and LG wrote the manuscript. BS, MG, RB, DB, JF, CF, EO, MM and LG contributed to patient recruitment and management. BS, JV, MM and LG extracted and analysed the data. BS performed statistical analyses. MM and LG supervised the project. All the authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval statement and patient consent statement
In conformity with the principles of the Helsinki declaration and according to the French Jardé law, written consent of the patients is not required in France for retrospective and observational non-interventional study.
Competing interests
The authors declare they have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sorin, B., Fadlallah, J., Garzaro, M. et al. Real-life use of mTOR inhibitor-based therapy in adults with autoimmune cytopenia highlights strong efficacy in relapsing/refractory multi-lineage autoimmune cytopenia. Ann Hematol 102, 2059–2068 (2023). https://doi.org/10.1007/s00277-023-05340-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05340-0