Abstract
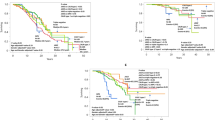
Approximately half of patients diagnosed with essential thrombocythemia (ET) are older adults (aged ≥ 60 years), but to date, little is known about the clinical and molecular characteristics of older patients diagnosed according to the 2016 World Health Organization criteria. We retrospectively collected clinical and molecular data from 282 older (≥ 60 years) and 621 younger ET patients (18–59 years) in China from March 1, 2012 to November 1, 2021 and summarized the clinical characteristics and treatment of these older ET patients. Compared to younger patients, older patients had a higher incidence of the JAK2V617F mutation (P = 0.001), a lower incidence of CALR mutations (P = 0.033) and a higher rate of epigenetic mutations (P < 0.001), TP53 mutations (P = 0.005), and RNA splicing mutations (P < 0.001). Older patients had not only a higher incidence of thrombosis but also a higher incidence of bleeding events. Furthermore, older patients had a significantly higher mortality rate after disease progression (P = 0.050) or after thrombotic events (P = 0.013). Risk factors for thrombosis or prognosis were significantly different between older patients and the entire ET cohort. In older patients, non-driver mutations contributed significantly to thrombotic complications and a poor prognosis, while the JAK2V617F mutation was a risk factor for overall survival but not for thrombotic events. The application of interferon in older ET patients was not inferior to that of hydroxyurea in terms of efficacy and safety. Older patients presented unique characteristics different from those of younger patients, which could provide new information for formulating more appropriate treatment and follow-up strategies.



Similar content being viewed by others
Data availability
The data sets generated and analyzed during the current study are available from the corresponding authors upon reasonable request.
References
Tefferi A, Barbui T (2019) Polycythemia vera and essential thrombocythemia: 2019 update on diagnosis, risk-stratification and management. Am J Hematol 94(1):133–143
Spivak JL (2017) Myeloproliferative Neoplasms. N Engl J Med 376(22):2168–2181
Vainchenker W, Kralovics R (2017) Genetic basis and molecular pathophysiology of classical myeloproliferative neoplasms. Blood 129(6):667–679
Tefferi A, Pardanani A (2019) Essential thrombocythemia. N Engl J Med 381(22):2135–2144
Szuber N et al (2019) 3023 Mayo clinic patients with myeloproliferative neoplasms: risk-stratified comparison of survival and outcomes data among disease Subgroups. Mayo Clin Proc 94(4):599–610
Tefferi A et al (2020) Mutation-enhanced international prognostic systems for essential thrombocythaemia and polycythaemia vera. Br J Haematol 189(2):291–302
Podoltsev NA et al (2019) Impact of hydroxyurea on survival and risk of thrombosis among older patients with essential thrombocythemia. J Natl Compr Canc Netw 17(3):211–219
Randi ML et al (2008) Hydroxyurea in old patients with essential thrombocythemia. Aging Clin Exp Res 20(4):376–380
Msaouel P et al (2014) Abnormal platelet count is an independent predictor of mortality in the elderly and is influenced by ethnicity. Haematologica 99(5):930–936
Barbui T et al (2012) Development and validation of an International Prognostic Score of thrombosis in World Health Organization-essential thrombocythemia (IPSET-thrombosis). Blood 120(26):5128–5133. quiz 5252
Haider M et al (2016) Validation of the revised International Prognostic Score of Thrombosis for Essential Thrombocythemia (IPSET-thrombosis) in 585 Mayo Clinic patients. Am J Hematol 91(4):390–934
Arber DA, Orazi A, Hasserjian R et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127(20):2391–2405, 128(3):462–463
Seguro FS et al (2020) Risk factors and incidence of thrombosis in a Brazilian cohort of patients with Philadelphia-negative myeloproliferative neoplasms. J Thromb Thrombolysis 49(4):667–672
Barbui T, Falanga A (2016) Molecular biomarkers of thrombosis in myeloproliferative neoplasms. Thromb Res 140(Suppl 1):S71-75
McMahon B, Stein BL (2013) Thrombotic and bleeding complications in classical myeloproliferative neoplasms. Semin Thromb Hemost 39(1):101–111
Barosi G et al (2013) Revised response criteria for polycythemia vera and essential thrombocythemia: an ELN and IWG-MRT consensus project. Blood 121(23):4778–4781
Auton A et al (2015) A global reference for human genetic variation. Nature 526(7571):68–74
Reumers J et al (2006) SNPeffect v2.0: a new step in investigating the molecular phenotypic effects of human non-synonymous SNPs. Bioinformatics 22(17): 2183–2185
Smigielski EM et al (2000) dbSNP: a database of single nucleotide polymorphisms. Nucleic Acids Res 28(1):352–355
Forbes SA et al (2008) The Catalogue of Somatic Mutations in Cancer (COSMIC). Curr Protoc Hum Genet. Chapter 10: p. Unit 10.11
Mesa RA et al (2017) NCCN guidelines insights: myeloproliferative neoplasms, version 2.2018. J Natl Compr Canc Netw 15(10): 1193–1207
Sun T, Zhang L (2013) Thrombosis in myeloproliferative neoplasms with JAK2V617F mutation. Clin Appl Thromb Hemost 19(4):374–381
Fu R et al (2014) External validation and clinical evaluation of the International Prognostic Score of Thrombosis for Essential Thrombocythemia (IPSET-thrombosis) in a large cohort of Chinese patients. Eur J Haematol 92(6):502–509
Nie YB et al (2018) ASXL1 mutations in Chinese patients with essential thrombocythemia. Exp Ther Med 15(5):4149–4156
Zhang L et al (2023) Clinical features and next-generation sequencing landscape of essential thrombocythemia, prefibrotic primary myelofibrosis, and overt fibrotic primary myelofibrosis: a Chinese monocentric retrospective study. J Cancer Res Clin Oncol 149(6):2383–2392
Cabagnols X et al (2015) Differential association of calreticulin type 1 and type 2 mutations with myelofibrosis and essential thrombocytemia: relevance for disease evolution. Leukemia 29(1):249–252
Tefferi A et al (2014) The prognostic advantage of calreticulin mutations in myelofibrosis might be confined to type 1 or type 1-like CALR variants. Blood 124(15):2465–2466
Segura-Díaz A et al (2020) Thrombotic risk detection in patients with polycythemia vera: The predictive role of DNMT3A/TET2/ASXL1 mutations. Cancers (Basel) 12(4):934
Stengel A et al (2021) Mutational patterns and their correlation to CHIP-related mutations and age in hematological malignancies. Blood Adv 5(21):4426–4434
Hautin M et al (2020) Splicing anomalies in myeloproliferative neoplasms: paving the way for new therapeutic venues. Cancers (Basel) 12(8):2216
Tefferi A et al (2016) Targeted deep sequencing in polycythemia vera and essential thrombocythemia. Blood Adv 1(1):21–30
Latorre E et al (2018) Mitochondria-targeted hydrogen sulfide attenuates endothelial senescence by selective induction of splicing factors HNRNPD and SRSF2. Aging (Albany NY) 10(7):1666–1681
Palandri F et al (2012) Bleeding in essential thrombocythaemia: a retrospective analysis on 565 patients. Br J Haematol 156(2):281–284
Finazzi G et al (2012) Incidence and risk factors for bleeding in 1104 patients with essential thrombocythemia or prefibrotic myelofibrosis diagnosed according to the 2008 WHO criteria. Leukemia 26(4):716–719
Alvarez-Larrán A et al (2016) Antiplatelet therapy versus observation in low-risk essential thrombocythemia with a CALR mutation. Haematologica 101(8):926–931
Tefferi A et al (2013) Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia 27(9):1874–1881
Passamonti F et al (2012) A prognostic model to predict survival in 867 World Health Organization-defined essential thrombocythemia at diagnosis: a study by the International Working Group on Myelofibrosis Research and Treatment. Blood 120(6):1197–1201
Acknowledgements
This project was supported by grants from the CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-073), the National Natural Science Foundation of China (81600099, 81970121, 82000136, 82270152, 82000127), National Key Research and Development Program of China (2019YFA0110802), Tianjin Municipal Science and Technology Commission Grant (18JCQNJC11900), CIFMS (2022-I2M-2-003, 2021-I2M-1-003), the Non-profit Central Research Institute Fund of the Chinese Academy of Medical Sciences (2020-PT310-011), and Haihe Laboratory of Cell Ecosystem Innovation Fund (HH22KYZX0022), and Clinical Research Fund of National Center for Clinical Medical Research of Hematology Diseases (2023NCRCA0109).
Funding
This project was supported by grants from the CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1–073), the National Natural Science Foundation of China (81600099, 81970121, 82000136, 82270152, 82000127), National Key Research and Development Program of China (2019YFA0110802), Tianjin Municipal Science and Technology Commission Grant (18JCQNJC11900), CIFMS (2022-I2M-2–003, 2021-I2M-1–003), the Non-profit Central Research Institute Fund of the Chinese Academy of Medical Sciences (2020-PT310-011), Haihe Laboratory of Cell Ecosystem Innovation Fund (22HHXBSS00022), and Clinical Research Fund of National Center for Clinical Medical Research of Hematology Diseases (2023NCRCA0109).
Author information
Authors and Affiliations
Contributions
RFF, HD, and DLZ contributed equally to this study and collected data, analyzed data, and wrote the paper. LZ and RCY designed the study, analyzed data, and reviewed the manuscript. TS, MKJ, and XYD collected data and analyzed data. XFL, FX, YFC, WL, XZ, YTH and HZ helped with data collection.
Corresponding authors
Ethics declarations
Ethics approval
This study has been approved by the Institutional Ethics Committee of each participating center.
Patient consent
This study obtained the informed written consent of the patients.
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rongfeng Fu, Huan Dong and Donglei Zhang should be regarded as cofirst authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, R., Dong, H., Zhang, D. et al. Clinical features and current treatment status of essential thrombocythemia in older adults: a multicenter real-world study in China. Ann Hematol 102, 2097–2107 (2023). https://doi.org/10.1007/s00277-023-05317-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05317-z