Abstract
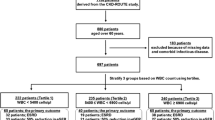
Chronic kidney disease (CKD) has a significant impact on sickle cell disease (SCD) morbidity and mortality. Early identification of individuals at highest risk of developing CKD may allow therapeutic intervention to prevent worse outcomes. This study aimed to evaluate the prevalence and risk factors for reduced estimated glomerular filtration rate (eGFR) among adults with SCD in Brazil. Participants in the REDS-III multicenter SCD cohort with more severe genotypes aged ≥ 18 years with at least two serum creatinine values were analyzed. The eGFR was calculated using the Jamaica Sickle Cell Cohort Study GFR equation. The eGFR categories were defined according to the K/DOQI. Participants with eGFR ≥ 90 were compared to those with those with eGFR < 90. Among the 870 participants, 647 (74.4%) had eGFR ≥ 90, 211 (24.3%) had eGFR 60 to 89, six (0.7%) had eGFR 30 to 59, and six (0.7%) had ESRD. Male sex (OR: 37.3; 95%CI: 22.4–65.1), higher age (OR: 1.04; 95%CI: 1.02–1.06), higher diastolic blood pressure (OR: 1.03; 95%CI: 1.009–1.06), lower Hb (OR: 0.80; 95%CI: 0.68–0.93), and lower reticulocytes (OR: 0.94; 95%CI: 0.89–0.99) levels were independently associated with eGFR < 90. There was a trend towards higher odds of death in participants with eGFR < 90 (OR: 1.8; 95%CI: 0.95–3.32; p = 0.065). In turn, participants with eGFR < 60 had a 12.2 (95%CI: 2.1–96.9) times higher odds for death when compared to those with eGFR ≥ 60. In this study, eGFR < 90 was observed in one-quarter of adults. Older age, male sex, higher diastolic blood pressure, lower hemoglobin, and lower reticulocyte levels were associated with occurrence of eGFR < 90. Estimated GFR < 60 increased the risk of mortality.
Similar content being viewed by others
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Piel FB, Steinberg MH, Rees DC (2017) Sickle cell disease. N Engl J Med 376(16):1561–1573. https://doi.org/10.1056/NEJMra1510865
Piel FB, Patil AP, Howes RE, Nyangiri OA, Gething PW, Dewi M, Temperley WH, Williams TN, Weatherall DJ, Hay SI (2013) Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates. Lancet 381(9861):142–151. https://doi.org/10.1016/S0140-6736(12)61229-X
Cançado RD, Jesus JA (2007) A doença falciforme no Brasil. Rev bras hematol hemoter 29(3):203–206
Kato GJ, Piel FB, Reid CD, Gaston MH, Ohene-Frempong K, Krishnamurti L, Smith WR, Panepinto JA, Weatherall DJ, Costa FF, Vichinsky EP (2018) Sickle cell disease. Nat Rev Dis Primers 4:18010. https://doi.org/10.1038/nrdp.2018.10
Malta DC, Machado ÍE, Pereira CA, Figueiredo AW, Aguiar LK, Almeida WDS, Souza MFM, Rosenfeld LG, Szwarcwald CL (2019) Evaluation of renal function in the Brazilian adult population, according to laboratory criteria from the National Health Survey. Revista brasileira de Epidemiol Brazilian J Epidemiol 22(Suppl 02):E190010. https://doi.org/10.1590/1980-549720190010.supl.2. (Supl. 090012)
Sharpe CC, Thein SL (2011) Sickle cell nephropathy - a practical approach. Br J Haematol 155(3):287–297. https://doi.org/10.1111/j.1365-2141.2011.08853.x
Ataga KI, Derebail VK, Archer DR (2014) The glomerulopathy of sickle cell disease. Am J Hematol 89(9):907–914. https://doi.org/10.1002/ajh.23762
Powars DR, Chan LS, Hiti A, Ramicone E, Johnson C (2005) Outcome of sickle cell anemia: a 4-decade observational study of 1056 patients. Medicine 84(6):363–376
Guasch A, Navarrete J, Nass K, Zayas CF (2006) Glomerular involvement in adults with sickle cell hemoglobinopathies: prevalence and clinical correlates of progressive renal failure. J Am Soc Nephrol 17(8):2228–2235. https://doi.org/10.1681/ASN.2002010084
Powars DR, Elliott-Mills DD, Chan L, Niland J, Hiti AL, Opas LM, Johnson C (1991) Chronic renal failure in sickle cell disease: risk factors, clinical course, and mortality. Ann Intern Med 115(8):614–620. https://doi.org/10.1097/01.md.0000189089.45003.52
Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, Klug PP (1994) Mortality in sickle cell disease. Life expectancy and risk factors for early death. The New England journal of medicine 330(23):1639–1644. https://doi.org/10.1056/NEJM199406093302303
Carneiro-Proietti ABF, Kelly S, Miranda Teixeira C, Sabino EC, Alencar CS, Capuani L, Salomon Silva TP, Araujo A, Loureiro P, Maximo C, Lobo C, Flor-Park MV, Rodrigues DOW, Mota RA, Goncalez TT, Hoppe C, Ferreira JE, Ozahata M, Page GP, Guo Y, Preiss LR, Brambilla D, Busch MP, Custer B, International Component of the NRE, Donor Evaluation S (2018) Clinical and genetic ancestry profile of a large multi-centre sickle cell disease cohort in Brazil. British journal of haematology 182(6):895–908. https://doi.org/10.1111/bjh.15462
Belisário AR, Carneiro-Proietti AB, Sabino EC, Araújo A, Loureiro P, Máximo C, Flor-Park MV, Rodrigues D, Ozahata MC, McClure C, Mota RA, Gomes Moura IC, Custer B, Kelly S (2020) Hb S/β-thalassemia in the REDS-III Brazil sickle cell disease cohort: clinical, laboratory and molecular characteristics. Hemoglobin 44(1):1–9. https://doi.org/10.1080/03630269.2020.1731530
Ballas SK, Lieff S, Benjamin LJ, Dampier CD, Heeney MM, Hoppe C, Johnson CS, Rogers ZR, Smith-Whitley K, Wang WC, Telen MJ, Investigators CSCC (2010) Definitions of the phenotypic manifestations of sickle cell disease. Am J Hematol 85(1):6–13. https://doi.org/10.1002/ajh.21550
de Martino CC, Alencar CS, Loureiro P, Carneiro-Proietti ABF, Maximo CA, Mota RA, Rodrigues DOW, Gaburo Junior N, Kelly S, Sabino EC, International Component of the NRE, Donor Evaluation S (2019) Use of an automated pyrosequencing technique for confirmation of sickle cell disease. PloS one 14(12):e0216020. https://doi.org/10.1371/journal.pone.0216020
Asnani MR, Lynch O, Reid ME (2013) Determining glomerular filtration rate in homozygous sickle cell disease: utility of serum creatinine based estimating equations. PloS one 8(7):e69922. https://doi.org/10.1371/journal.pone.0069922
Inker LA, Eneanya ND, Coresh J, Tighiouart H, Wang D, Sang Y, Crews DC, Doria A, Estrella MM, Froissart M, Grams ME, Greene T, Grubb A, Gudnason V, Gutiérrez OM, Kalil R, Karger AB, Mauer M, Navis G, Nelson RG, Poggio ED, Rodby R, Rossing P, Rule AD, Selvin E, Seegmiller JC, Shlipak MG, Torres VE, Yang W, Ballew SH, Couture SJ, Powe NR, Levey AS (2021) New creatinine- and cystatin C-based equations to estimate GFR without race. N Engl J Med 385(19):1737–1749. https://doi.org/10.1056/NEJMoa2102953
K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification (2002) American journal of kidney diseases : the official journal of the National Kidney Foundation 39 (2 Suppl 1):S1–266
Stevens PE, Levin A (2013) Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 158(11):825–830. https://doi.org/10.7326/0003-4819-158-11-201306040-00007
Gosmanova EO, Zaidi S, Wan JY, Adams-Graves PE (2014) Prevalence and progression of chronic kidney disease in adult patients with sickle cell disease. J Investig Med : Off Publ Am Fed Clin Res 62(5):804–807. https://doi.org/10.1097/01.JIM.0000446836.75352.72
Asnani MR, Reid ME (2015) Renal function in adult Jamaicans with homozygous sickle cell disease. Hematology 20(7):422–428. https://doi.org/10.1179/1607845414Y.0000000213
Saraf SL, Shah BN, Zhang X, Han J, Tayo BO, Abbasi T, Ostrower A, Guzman E, Molokie RE, Gowhari M, Hassan J, Jain S, Cooper RS, Machado RF, Lash JP, Gordeuk VR (2017) APOL1, alpha-thalassemia, and BCL11A variants as a genetic risk profile for progression of chronic kidney disease in sickle cell anemia. Haematologica 102(1):e1–e6. https://doi.org/10.3324/haematol.2016.154153
McClellan AC, Luthi JC, Lynch JR, Soucie JM, Kulkarni R, Guasch A, Huff ED, Gilbertson D, McClellan WM, DeBaun MR (2012) High one year mortality in adults with sickle cell disease and end-stage renal disease. Br J Haematol 159(3):360–367. https://doi.org/10.1111/bjh.12024
Kato GJ, Gladwin MT, Steinberg MH (2007) Deconstructing sickle cell disease: reappraisal of the role of hemolysis in the development of clinical subphenotypes. Blood Rev 21(1):37–47. https://doi.org/10.1016/j.blre.2006.07.001
Nath KA, Katusic ZS (2012) Vasculature and kidney complications in sickle cell disease. J Am Soc Nephrol 23(5):781–784. https://doi.org/10.1681/ASN.2011101019
Asnani M, Serjeant G, Royal-Thomas T, Reid M (2016) Predictors of renal function progression in adults with homozygous sickle cell disease. Br J Haematol 173(3):461–468. https://doi.org/10.1111/bjh.13967
McKie KT, Hanevold CD, Hernandez C, Waller JL, Ortiz L, McKie KM (2007) Prevalence, prevention, and treatment of microalbuminuria and proteinuria in children with sickle cell disease. J Pediatr Hematol Oncol 29(3):140–144. https://doi.org/10.1097/MPH.0b013e3180335081
Belisario AR, de Almeida JA, Mendes FG, da Silva DMM, Planes W, Rezende PV, Silva CM, Brito AC, Sales RR, Viana MB, Simoes ESAC (2020) Prevalence and risk factors for albuminuria and glomerular hyperfiltration in a large cohort of children with sickle cell anemia. Am J Hematol 95(5):E125–E128. https://doi.org/10.1002/ajh.25763
Geard A, Pule GD, ChetchaChemegni B, Ngo Bitoungui VJ, Kengne AP, Chimusa ER, Wonkam A (2017) Clinical and genetic predictors of renal dysfunctions in sickle cell anaemia in Cameroon. Br J Haematol 178(4):629–639. https://doi.org/10.1111/bjh.14724
Roger C, Lionnet F, Mattioni S, Livrozet M, Steichen O, Letavernier E, Hammoudi N, Avellino V, Haymann JP (2021) Risk factors for CKD stage II onset in a prospective cohort of homozygous sickle cell adults. Am J Hematol. https://doi.org/10.1002/ajh.26264
Konukoglu D, Uzun H (2017) Endothelial dysfunction and hypertension. Adv Exp Med Biol 956:511–540. https://doi.org/10.1007/5584_2016_90
Wang WC, Ware RE, Miller ST, Iyer RV, Casella JF, Minniti CP, Rana S, Thornburg CD, Rogers ZR, Kalpatthi RV, Barredo JC, Brown RC, Sarnaik SA, Howard TH, Wynn LW, Kutlar A, Armstrong FD, Files BA, Goldsmith JC, Waclawiw MA, Huang X, Thompson BW, investigators BH (2011) Hydroxycarbamide in very young children with sickle-cell anaemia: a multicentre, randomised, controlled trial (BABY HUG). Lancet 377(9778):1663–1672. https://doi.org/10.1016/S0140-6736(11)60355-3
Afangbedji N, Jerebtsova M (2022) Glomerular filtration rate abnormalities in sickle cell disease. Front Med (Lausanne) 9:1029224. https://doi.org/10.3389/fmed.2022.1029224
da Silva MC, Zuccherato LW, Lucena FC, Soares-Souza GB, Vieira ZM, Pena SD, Martins ML, Tarazona-Santos E (2011) Extensive admixture in Brazilian sickle cell patients: implications for the mapping of genetic modifiers. Blood 118(16):4493–4495. https://doi.org/10.1182/blood-2011-06-361915. (author reply 4495)
Jara JMC, Fonseca GHH, Caldin B, Marques KS, Buchpiguel CA, Rocha VG, Menosi SFG (2020) TAXA DE FILTRAÇÃO GLOMERULAR AVALIADA POR TÉCNICA DE MEDICINA NUCLEAR: MEDIDA DE EDTA MARCADO COM CROMO-51 EM PACIENTES ADULTOS COM DOENÇA FALCIFORME (SS E SΒ0 TALASSEMIA) E MARCADORES DE GRAVIDADE DA DOENÇA DE BASE. Hematol Transfusion Cell Therapy 42:14–15. https://doi.org/10.1016/j.htct.2020.10.024
Acknowledgements
First, the authors acknowledge all participants and parents of pediatric participants for their cooperation in being part of this the study. The authors also thank the staff at all participating Brazilian and American research sites. Without all of these contributions, this study would not have been possible. This work was supported by the NHLBI Recipient Epidemiology and Donor Evaluation Study-III: International Component (Brazil), with the participation of the following centers and investigators. Brazilian participants: Instituto de Medicina Tropical de São Paulo (USP)—Ester C. Sabino, Cecilia Alencar; Fundação Pró-Sangue (São Paulo)—Alfredo Mendrone Jr., Cesar de Almeida Neto, Ligia Capuani; Instituto de Tratamento do Câncer Infantil (São Paulo)—Miriam Park; Faculdade de Medicina da Universidade de São Paulo (São Paulo)—Paula Blatyta; Hemominas—Belo Horizonte (Minas Gerais)—Anna Bárbara de Freitas Carneiro-Proietti, Carolina Miranda Teixeira, Tassila Salomon, Franciane Mendes de Oliveira, Valquíria Reis; Hemominas, Montes Claros (Minas Gerais)—Rosemere Afonso Mota, José Wilson Sales; Hemominas—Juiz de Fora (Minas Gerais)—Daniela de Oliveira Werneck; Fundação Hemope – Recife (Pernambuco)—Paula Loureiro, Aderson Araújo, Maria do Carmo Valgueir; Hemorio (Rio de Janeiro)—Clarisse Lobo, Claudia Maximo; Instituto de Matemática e Estatística da Universidade de São Paulo—USP (São Paulo)—João Eduardo Ferreira, Márcio Katsumi Oikawa, Pedro Losco Takecian, Mina Cintho Ozahata, Rodrigo Muller de Carvalho. US investigators: Vitalant Research Institute and University of California San Francisco—Brian Scott Custer, Michael P. Busch, Shannon Kelly and Thelma Therezinha Gonçalez; RTI—Research Triangle Institute—Donald Brambilla, Liliana RPreiss, Christopher McClure; UCSF Benioff Children’s Hospital Oakland—Carolyn Hoppe; National Heart, Lung, and Blood Institute, NIH—Simone A. Glynn.
Funding
The Recipient Epidemiology and Donor Evaluation Study (REDS-III Brazil) was supported by the National Institutes of Health, National Heart, Lung, and Blood Institute under contracts HHSN268201100007I. André Rolim Belisário received a scholarship from the International Traineeships in AIDS Prevention Studies program (ITAPS) to participate in a scientific manuscript writing program at University of California, San Francisco.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Belisário, A.R., Simões e Silva, A.C., Moura, I.C.G. et al. Estimated glomerular filtration rate in Brazilian adults with sickle cell disease: results from the REDS-III multicenter cohort study. Ann Hematol 102, 1019–1027 (2023). https://doi.org/10.1007/s00277-023-05150-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05150-4