Abstract
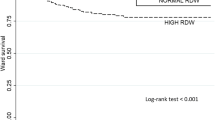
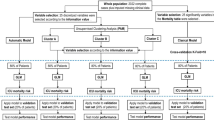
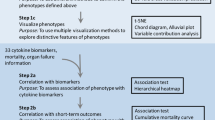
Sickle cell disease (SCD) is associated with multiple known complications and increased mortality. This study aims to further understand the profile of intensive care unit (ICU) admissions of SCD patients. In this single-center retrospective cohort (approval number 0926–11), we evaluated SCD-related ICU admissions at our hospital in São Paulo, Brazil. Admissions were clustered using clinical data and organ dysfunction at ICU admission. A hierarchical clustering method was used to distinguish phenotypes. From 140 admissions obtained, 125 were included. The mean age was 30 years, 48% were male, and SS genotype was predominant (71.2%). Non-surgical causes of admissions accounted for 85.6% (n = 107). The mean Sequential Organ Failure Assessment score (SOFA) was 4 (IQR 2–7). Vasopressors were required by 12% and mechanical ventilation by 17.6%. After analysis of the average silhouette width, the optimal number of clusters was 3: cluster 1 (n = 69), cluster 2 (n = 25), cluster 3 (n = 31). Cluster 1 had a mean age of 29 years, 87% of SS genotype, and mean SOFA of 4. Cluster 2 had a mean age of 37 years, 80% of SS genotype, and mean SOFA of 8. Cluster 3 had a mean age of 26 years, 29% of SS genotype, and mean SOFA of 3. The need for mechanical ventilation was 11.6%, 44%, and 9.7%, respectively. Mortality was significantly higher in cluster 2 (44%, p = 0.012). This cohort of critical SCD admissions suggested the presence of three different profiles. This can be informative in the ICU setting to identify SCD patients at higher risk of worse outcomes.


Similar content being viewed by others
References
Hamideh D, Alvarez O (2013) Sickle cell disease related mortality in the United States (1999–2009). Pediatr Blood Cancer 60(9):1482–1486
Maitra P, Caughey M, Robinson L, Desai PC, Jones S, Nouraie M, Gladwin MT, Hinderliter A, Cai J, Ataga KI (2017) Risk factors for mortality in adult patients with sickle cell disease: a meta-analysis of studies in North America and Europe. Haematologica 102(4):626–636
Gardner K, Bell C, Bartram JL, Allman M, Awogbade M, Rees DC, Ervine M, Thein SL (2010) Outcome of adults with sickle cell disease admitted to critical care - experience of a single institution in the UK. Br J Haematol 150(5):610–613
Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, Klug PP (1994) Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med 330(23):1639–1644
Cecchini J, Lionnet F, Djibre M, Parrot A, Stojanovic KS, Girot R, Fartoukh M (2014) Outcomes of adult patients with sickle cell disease admitted to the ICU: a case series*. Crit Care Med 42(7):1629–1639
Al Khawaja SA, Ateya ZM, Al Hammam RA (2017) predictors of mortality in adults with sickle cell disease admitted to intensive care unit in Bahrain. J Crit Care 42:238–242
Castela Forte J, Perner A, van der Horst ICC (2019) The use of clustering algorithms in critical care research to unravel patient heterogeneity. Intensive Care Med 45(7):1025–1028
Zampieri FG, Costa EL, Iwashyna TJ, Carvalho CRR, Damiani LP, Taniguchi LU, Amato MBP, Cavalcanti AB (2019) Alveolar recruitment for acute respiratory distress syndrome trial I: heterogeneous effects of alveolar recruitment in acute respiratory distress syndrome: a machine learning reanalysis of the alveolar recruitment for acute respiratory distress syndrome Trial. Br J Anaesth 123(1):88–95
Miailhe AF, Mercier E, Maamar A, Lacherade JC, Le Thuaut A, Gaultier A, Asfar P, Argaud L, Ausseur A, Ben Salah A et al (2019) Severe leptospirosis in non-tropical areas: a nationwide, multicentre, retrospective study in French ICUs. Intensive Care Med 45(12):1763–1773
d’Humieres T, Savale L, Inamo J, Deux JF, Deswarte S, Lionnet F, Loko G, Chantalat C, Damy T, Guillet H et al (2021) Cardiovascular phenotypes predict clinical outcomes in sickle cell disease: an echocardiography-based cluster analysis. Am J Hematol 96(9):1166–1175
Mohammed A, Podila PSB, Davis RL, Ataga KI, Hankins JS, Kamaleswaran R (2020) Using machine learning to predict early onset acute organ failure in critically ill intensive care unit patients with sickle cell disease: retrospective study. J Med Internet Res 22(5):e14693
Metnitz PG, Moreno RP, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR et al (2005) SAPS 3–from evaluation of the patient to evaluation of the intensive care unit. Part 1: Objectives, methods and cohort description. Intensive Care Med 31(10):1336–1344
Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR et al (2005) SAPS 3–from evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med 31(10):1345–1355
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22(7):707–710
Chen LM, Kennedy EH, Sales A, Hofer TP (2013) Use of health IT for higher-value critical care. N Engl J Med 368(7):594–597
Vranas KC, Jopling JK, Sweeney TE et al (2017) Identifying distinct subgroups of ICU patients: a machine learning approach. Crit Care Med 45(10):1607–1615
Dlugacz YD, Stier L, Lustbader D, Jacobs MC, Hussain E, Greenwood A (2002) Expanding a performance improvement initiative in critical care from hospital to system. Jt Comm J Qual Improv 28(8):419–434
Silva-Pinto AC, Alencar de Queiroz MC, AntoniazzoZamaro PJ, Arruda M, Pimentel Dos Santos H (2019) The Neonatal Screening Program in Brazil, focus on sickle cell disease (SCD). Int J Neonatal Screen. 5(1):11 (Published 2019 Jan 26)
Santo AH (2022) Sickle cell disease related mortality in Brazil, 2000–2018. Hematol Transfus Cell Ther 44(2):177–185
Castro O, Brambilla DJ, Thorington B et al (1994) The acute chest syndrome in sickle cell disease: incidence and risk factors. The Cooperative Study of Sickle Cell Disease. Blood. 84(2):643–649
Carneiro-Proietti ABF, Kelly S, Miranda Teixeira C et al (2018) Clinical and genetic ancestry profile of a large multi-centre sickle cell disease cohort in Brazil. Br J Haematol 182(6):895–908. https://doi.org/10.1111/bjh.15462
Tawfic QA, Kausalya R, Al-Sajee D, Burad J, Mohammed AK, Narayanan A (2012) Adult sickle cell disease: a five-year experience of intensive care management in a University Hospital in Oman. Sultan Qaboos Univ Med J 12(2):177–183
Yawn BP, Buchanan GR, Afenyi-Annan AN et al (2014) Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members [published correction appears in JAMA. 2014 Nov 12;312(18):1932] [published correction appears in JAMA. 2015 Feb 17;313(7):729]. JAMA 312(10):1033–1048
da Guarda CC, Yahouédéhou SCMA, Santiago RP et al (2020) Sickle cell disease: a distinction of two most frequent genotypes (HbSS and HbSC). PLoS One. 15(1):e0228399 (Published 2020 Jan 29)
Darbari DS, Kple-Faget P, Kwagyan J, Rana S, Gordeuk VR, Castro O (2006) Circumstances of death in adult sickle cell disease patients. Am J Hematol 81(11):858–863
Author information
Authors and Affiliations
Contributions
First draft: all authors.
Conception: E. M. H. P., L. U. T., G. H. H. F.
Statistical analysis: L. U. T.
Interpretation of results: E. M. H. P., L. U. T., B. B., A. M.
Approval of final version: all authors.
Corresponding author
Ethics declarations
Ethical approval
This study was carried out at Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Padrão, E.M.H., Bustos, B., Mahesh, A. et al. Phenotypes of sickle cell intensive care admissions: an unsupervised machine learning approach in a single-center retrospective cohort. Ann Hematol 101, 1951–1957 (2022). https://doi.org/10.1007/s00277-022-04918-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04918-4