Abstract
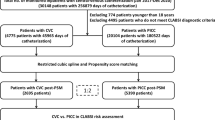
Peripherally inserted central venous catheters (PICCs) have a potential advantage in preventing central line-associated bloodstream infection (CLABSI) compared with the centrally inserted ones (CICCs). However, due to a limited number of studies with insufficient statistical evaluation, the superiority of PICCs is difficult to be generalized in adult hematology unit. We conducted a single-center retrospective study and compared the risk of CLABSI between 472 CICCs and 557 PICCs inserted in adult patients with hematological disorders through conventional multivariate models and a propensity score-adjusted analysis. The overall CLABSI incidence in CICCs and PICCs was 5.11 and 3.29 per 1000 catheter days (P = 0.024). The multivariate Cox regression analysis (hazard ratio [HR]: 0.48; 95% confidence interval [CI]: 0.31–0.75; P = 0.001) and Fine-Gray subdistribution analysis (HR: 0.59; 95% CI: 0.37–0.93; P = 0.023) demonstrated that PICC was independently associated with a reduced risk of CLABSI. Moreover, the stabilized inverse probability of treatment weighting analysis, which further reduced the selection bias between CICCs and PICCs, showed that PICCs significantly prevented CLABSI (HR: 0.58; 95% CI: 0.35–0.94; P = 0.029). Microbiologically, PICCs showed a significant decrease in gram-positive cocci (P = 0.001) and an increase in gram-positive bacilli (P = 0.002) because of a remarkable reduction in Staphylococci and increase in Corynebacterium species responsible for CLABSI. Our study confirmed that PICC was a superior alternative to CICC in preventing CLABSI in the adult hematology unit, while it posed a microbiological shift in local epidemiology.

Similar content being viewed by others
Data availability
The dataset analyzed in the current study is available from the corresponding authors on reasonable request.
Change history
12 July 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00277-022-04927-3
References
Blot SI, Depuydt P, Annemans L, Benoit D, Hoste E, De Waele JJ, Decruyenaere J, Vogelaers D, Colardyn F, Vandewoude KH (2005) Clinical and economic outcomes in critically ill patients with nosocomial catheter-related bloodstream infections. Clin Infect Dis 41:1591–1598. https://doi.org/10.1086/497833
Stone PW, Braccia D, Larson E (2005) Systematic review of economic analyses of health care-associated infections. Am J Infect Control 33:501–509. https://doi.org/10.1016/j.ajic.2005.04.246
Higuera F, Rangel-Frausto MS, Rosenthal VD, Soto JM, Castañon J, Franco G, Tabal-Galan N, Ruiz J, Duarte P, Graves N (2007) Attributable cost and length of stay for patients with central venous catheter-associated bloodstream infection in Mexico City intensive care units: a prospective, matched analysis. Infect Control Hosp Epidemiol 28:31–35. https://doi.org/10.1086/510812
Chopra V, O’Horo JC, Rogers MA, Maki DG, Safdar N (2013) The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 34:908–918. https://doi.org/10.1086/671737
Mollee P, Jones M, Stackelroth J, van Kuilenburg R, Joubert W, Faoagali J, Looke D, Harper J, Clements A (2011) Catheter-associated bloodstream infection incidence and risk factors in adults with cancer: a prospective cohort study. J Hosp Infect 78:26–30. https://doi.org/10.1016/j.jhin.2011.01.018
Sakai T, Kohda K, Konuma Y, Hiraoka Y, Ichikawa Y, Ono K, Horiguchi H, Tatekoshi A, Takada K, Iyama S, Kato J (2014) A role for peripherally inserted central venous catheters in the prevention of catheter-related blood stream infections in patients with hematological malignancies. Int J Hematol 100:592–598. https://doi.org/10.1007/s12185-014-1677-9
Fracchiolla NS, Todisco E, Bilancia A, Gandolfi S, Orofino N, Guidotti F, Mancini V, Marbello L, Assanelli A, Bernardi M, Santoro A, Cairoli R, Consonni D, Cortelezzi A (2017) Clinical management of peripherally inserted central catheters compared to conventional central venous catheters in patients with hematological malignancies: a large multicenter study of the REL GROUP (Rete Ematologica Lombarda - Lombardy Hematologic Network, Italy). Am J Hematol 92:E656–E659. https://doi.org/10.1002/ajh.24903
Lee JH, Kim ET, Shim DJ, Kim IJ, Byeon JH, Lee IJ, Kim HB, Choi YJ, Lee JH (2019) Prevalence and predictors of peripherally inserted central catheter-associated bloodstream infections in adults: a multicenter cohort study. PLoS ONE 14:e0213555. https://doi.org/10.1371/journal.pone.0213555
Picardi M, Della Pepa R, Cerchione C, Pugliese N, Mortaruolo C, Trastulli F, Giordano C, Grimaldi F, Zacheo I, Raimondo M, Chiurazzi F, Pane F (2019) A frontline approach with peripherally inserted versus centrally inserted central venous catheters for remission induction chemotherapy phase of acute myeloid leukemia: a randomized comparison. Clin Lymphoma Myeloma Leuk 19:e184–e194. https://doi.org/10.1016/j.clml.2018.12.008
Baier C, Linke L, Eder M, Schwab F, Chaberny IF, Vonberg RP, Ebadi E (2020) Incidence, risk factors and healthcare costs of central line-associated nosocomial bloodstream infections in hematologic and oncologic patients. PLoS ONE 15:e0227772. https://doi.org/10.1371/journal.pone.0227772
Mollee P, Okano S, Abro E, Looke D, Kennedy G, Harper J, Clouston J, Van Kuilenburg R, Geary A, Joubert W, Eastgate M, Jones M (2020) Catheter-associated bloodstream infections in adults with cancer: a prospective randomized controlled trial. J Hosp Infect 106:335–342. https://doi.org/10.1016/j.jhin.2020.07.021
Hashimoto Y, Hosoda R, Omura H, Tanaka T (2021) Catheter-related bloodstream infection associated with multiple insertions of the peripherally inserted central catheter in patients with hematological disorders. Sci Rep 11:12209. https://doi.org/10.1038/s41598-021-91749-4
Safdar N, Maki DG (2005) Risk of catheter-related bloodstream infection with peripherally inserted central venous catheters used in hospitalized patients. Chest 128:489–495. https://doi.org/10.1378/chest.128.2.489
Maki DG, Kluger DM, Crnich CJ (2006) The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc 81:1159–1171. https://doi.org/10.4065/81.9.1159
Mavrovounis G, Mermiri M, Chatzis DG, Pantazopoulos I (2020) Peripherally inserted central catheter lines for intensive care unit and onco-hematologic patients: a systematic review and meta-analysis. Heart Lung 49:922–933. https://doi.org/10.1016/j.hrtlng.2020.07.008
Luo X, Guo Y, Yu H, Li S, Yin X (2017) Effectiveness, safety and comfort of StatLock securement for peripherally-inserted central catheters: a systematic review and meta-analysis. Nurs Health Sci 19:403–413. https://doi.org/10.1111/nhs.12361
Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O’Grady NP, Pettis AM, Rupp ME, Sandora T, Maragakis LL, Yokoe DS, Society for Healthcare Epidemiology of A (2014) Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 35:753–771. https://doi.org/10.1086/676533
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332. https://doi.org/10.1016/j.ajic.2008.03.002
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 34:3661–3679. https://doi.org/10.1002/sim.6607
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Austin PC, Lee DS, Fine JP (2016) Introduction to the analysis of survival data in the presence of competing risks. Circulation 133:601–609. https://doi.org/10.1161/CIRCULATIONAHA.115.017719
Carter JH, Langley JM, Kuhle S, Kirkland S (2016) Risk factors for central venous catheter-associated bloodstream infection in pediatric patients: a cohort study. Infect Control Hosp Epidemiol 37:939–945. https://doi.org/10.1017/ice.2016.83
Weber S, von Cube M, Sommer H, Wolkewitz M (2016) Necessity of a competing risk approach in risk factor analysis of central line-associated bloodstream infection. Infect Control Hosp Epidemiol 37:1255–1257. https://doi.org/10.1017/ice.2016.166
Kuhle S, Carter JH, Kirkland S, Langley JM, Maguire B, Smith B (2017) Reply to Weber, von Cube, Sommer, Wolkewitz: Necessity of a competing risk approach in risk factor analysis of central-line-associated bloodstream infection. Infect Control Hosp Epidemiol 38:511. https://doi.org/10.1017/ice.2016.331
Schears GJ, Ferko N, Syed I, Arpino JM, Alsbrooks K (2021) Peripherally inserted central catheters inserted with current best practices have low deep vein thrombosis and central line-associated bloodstream infection risk compared with centrally inserted central catheters: a contemporary meta-analysis. J Vasc Access 22:9–25. https://doi.org/10.1177/1129729820916113
Skowron K, Bauza-Kaszewska J, Kraszewska Z, Wiktorczyk-Kapischke N, Grudlewska-Buda K, Kwiecinska-Pirog J, Walecka-Zacharska E, Radtke L, Gospodarek-Komkowska E (2021) Human skin microbiome: impact of intrinsic and extrinsic factors on skin microbiota. Microorganisms 9:543. https://doi.org/10.3390/microorganisms9030543
Waterhouse J, Bandisode V, Brandon D, Olson M, Docherty SL (2014) Evaluation of the use of a stabilization device to improve the quality of care in patients with peripherally inserted central catheters. AACN Adv Crit Care 25:213–220. https://doi.org/10.1097/nci.0000000000000026
Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, Sexton B, Hyzy R, Welsh R, Roth G, Bander J, Kepros J, Goeschel C (2006) An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med 355:2725–2732. https://doi.org/10.1056/NEJMoa061115
Ista E, van der Hoven B, Kornelisse RF, van der Starre C, Vos MC, Boersma E, Helder OK (2016) Effectiveness of insertion and maintenance bundles to prevent central-line-associated bloodstream infections in critically ill patients of all ages: a systematic review and meta-analysis. Lancet Infect Dis 16:724–734. https://doi.org/10.1016/s1473-3099(15)00409-0
Ray-Barruel G, Xu H, Marsh N, Cooke M, Rickard CM (2019) Effectiveness of insertion and maintenance bundles in preventing peripheral intravenous catheter-related complications and bloodstream infection in hospital patients: a systematic review. Infect Dis Health 24:152–168. https://doi.org/10.1016/j.idh.2019.03.001
Woods-Hill CZ, Papili K, Nelson E, Lipinski K, Shea J, Beidas R, Lane-Fall M (2021) Harnessing implementation science to optimize harm prevention in critically ill children: A pilot study of bedside nurse CLABSI bundle performance in the pediatric intensive care unit. Am J Infect Control 49:345–351. https://doi.org/10.1016/j.ajic.2020.08.019
Lin KY, Cheng A, Chang YC, Hung MC, Wang JT, Sheng WH, Hseuh PR, Chen YC, Chang SC (2017) Central line-associated bloodstream infections among critically-ill patients in the era of bundle care. J Microbiol Immunol Infect 50:339–348. https://doi.org/10.1016/j.jmii.2015.07.001
Lendak D, Puerta-Alcalde P, Moreno-Garcia E, Chumbita M, Garcia-Pouton N, Cardozo C, Morata L, Suarez-Lledo M, Hernandez-Meneses M, Ghiglione L, Marco F, Martinez JA, Mensa J, Urosevic I, Soriano A, Garcia-Vidal C (2021) Changing epidemiology of catheter-related bloodstream infections in neutropenic oncohematological patients. PLoS ONE 16:e0251010. https://doi.org/10.1371/journal.pone.0251010
Puerta-Alcalde P, Cardozo C, Marco F, Suarez-Lledo M, Moreno E, Morata L, Fernandez-Aviles F, Gutierrez-Garcia G, Chumbita M, Rosinol L, Martinez JA, Martinez C, Mensa J, Urbano A, Rovira M, Soriano A, Garcia-Vidal C (2020) Changing epidemiology of bloodstream infection in a 25-years hematopoietic stem cell transplant program: current challenges and pitfalls on empiric antibiotic treatment impacting outcomes. Bone Marrow Transplant 55:603–612. https://doi.org/10.1038/s41409-019-0701-3
Rodriguez-Creixems M, Munoz P, Martin-Rabadan P, Cercenado E, Guembe M, Bouza E (2013) Evolution and aetiological shift of catheter-related bloodstream infection in a whole institution: the microbiology department may act as a watchtower. Clin Microbiol Infect 19:845–851. https://doi.org/10.1111/1469-0691.12050
Marcos M, Soriano A, Inurrieta A, Martinez JA, Romero A, Cobos N, Hernandez C, Almela M, Marco F, Mensa J (2011) Changing epidemiology of central venous catheter-related bloodstream infections: increasing prevalence of Gram-negative pathogens. J Antimicrob Chemother 66:2119–2125. https://doi.org/10.1093/jac/dkr231
Abe M, Kimura M, Maruyama H, Watari T, Ogura S, Takagi S, Uchida N, Otsuka Y, Taniguchi S, Araoka H (2021) Clinical characteristics and drug susceptibility patterns of Corynebacterium species in bacteremic patients with hematological disorders. Eur J Clin Microbiol Infect Dis 40:2095–2104. https://doi.org/10.1007/s10096-021-04257-8
Silva-Santana G, Silva CMF, Olivella JGB, Silva IF, Fernandes LMO, Sued-Karam BR, Santos CS, Souza C, Mattos-Guaraldi AL (2021) Worldwide survey of Corynebacterium striatum increasingly associated with human invasive infections, nosocomial outbreak, and antimicrobial multidrug-resistance, 1976–2020. Arch Microbiol 203:1863–1880. https://doi.org/10.1007/s00203-021-02246-1
Yamamuro R, Hosokawa N, Otsuka Y, Osawa R (2021) Clinical characteristics of Corynebacterium bacteremia caused by different species Japan 2014–2020. Emerg Infect Dis 27(12):2981–2987. https://doi.org/10.3201/eid2712.210473.
Barberis CM, Sandoval E, Rodriguez CH, Ramírez MS, Famiglietti A, Almuzara M, Vay C (2018) Comparison between disk diffusion and agar dilution methods to determine in vitro susceptibility of Corynebacterium spp. clinical isolates and update of their susceptibility. J Glob Antimicrob Resist 14:246–252. https://doi.org/10.1016/j.jgar.2018.05.009
See I, Iwamoto M, Allen-Bridson K, Horan T, Magill SS, Thompson ND (2013) Mucosal barrier injury laboratory-confirmed bloodstream infection: results from a field test of a new National Healthcare Safety Network definition. Infect Control Hosp Epidemiol 34:769–776. https://doi.org/10.1086/671281
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YN and MI analyzed the clinical data and drafted the manuscript, figures, and tables. MI and MS formed an infection control team with specific qualifications for central line management and collected clinical, microbiological, and CLABSI data. KS, NY, MT, MY, TY, YH, TN, and TY interpreted data and revised the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The Ethics Committee of Osaka City General Hospital approved the protocol of this study (protocol file number: 2009096). All procedures were followed in accordance with the ethical standards of the responsible committee and the Helsinki Declaration.
Consent to participate
Informed consent from participants was obtained in the form of opt-outs on the institutional website because this study was retrospective and used anonymized data.
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: This article was originally published with an incorrect table presentation in table 3.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakaya, Y., Imasaki, M., Shirano, M. et al. Peripherally inserted central venous catheters decrease central line-associated bloodstream infections and change microbiological epidemiology in adult hematology unit: a propensity score-adjusted analysis. Ann Hematol 101, 2069–2077 (2022). https://doi.org/10.1007/s00277-022-04908-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04908-6