Abstract
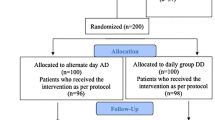
Iron-deficiency anemia (IDA) is accepted as the most common cause of anemia in the world. The main goals of iron replacement therapy are to normalize the hemoglobin level and to replace iron stores. Current guidelines for treating iron deficiency recommend daily divided doses of iron to increase absorption. Hepcidin is a key regulator of systemic iron balance and acts in harmony with intracellular iron metabolism. Daily dosing and divided doses may increase serum hepcidin and decrease iron absorption. In this study, it was aimed to compare the effectiveness of daily and every other day oral iron replacement therapy in women of reproductive age with iron-deficiency anemia. We included premenopausal female patients aged between 18 and 50 years with iron-deficiency anemia. Forty patients were given oral iron therapy at a daily dose of 2*80 mg (iron sulfate). Forty-three patients were given iron treatment at a dose of 2*80 mg (iron sulfate) every other day. After 2 months of oral iron therapy, there was a significant improvement in hemoglobin, mean corpuscular volume, serum iron, total iron-binding capacity, and transferrin saturation in both groups. The values of hemoglobin, serum iron, transferrin saturation, and ferritin significantly increased at the end of the treatment for both groups. Although the median hepcidin level on the 15th-day measurement in the every other day treatment group was higher than that in the daily treatment group, there was no significant difference. As a result, the patients’ compliance with the treatment can be increased by offering treatment every other day instead of daily, since it provides similar treatment effectiveness.

Similar content being viewed by others
References
Vos T, Abajobir AA, Abate KH et al (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:1211–1259
World Health Organization (2021) Anaemia in women and children: WHO global anaemia estimates, 2021st edn. World Health Organization, Geneva
Cook JD (2005) Diagnosis and management of iron-deficiency anaemia. Best Pract Res Clin Haematol 18(2):319–332
Taha A, Azhar S, Lone T et al (2014) Iron deficiency anaemia in reproductive age women attending obstetrics and gynecology outpatient of university health centre in Al-ahsa, Saudi Arabia. Afr J Tradit Complement Altern Med 11(2):339–342
Stoffel NU, Cercamondi CI, Brittenham G, Zeder C, Geurts-Moespot AJ, Swinkels DW, Moretti D, Zimmermann MB (2017) Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials. Lancet Haematol 4(11):e524–e533
Snook J, Bhala N, Beales Ian L P et al (2021) British Society of Gastroenterology guidelines for the management of iron deficiency anaemia in adults. Gut 70(11):2030–2051
Moretti D, Goede JS, Zeder C, Jiskra M, Chatzinakou V, Tjalsma H, Melse-Boonstra A, Brittenham G, Swinkels DW, Zimmermann MB (2015) Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood 126(17):1981–1989
Oflas ND, Demircioğlu S, Doğan NY, Eker E, Kutlucan A, Doğan A, Aslan M, Demir C (2020) Comparison of the effects of oral iron treatment every day and every other day in female patients with iron deficiency anaemia. Intern Med J 50(7):854–858
Nemeth E, Rivera S, Gabayan V et al (2004) IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Invest 113(9):1271–1276
Lin L, Valore EV, Nemeth E, Goodnough JB, Gabayan V, Ganz T (2007) Iron transferrin regulates hepcidin synthesis in primary hepatocyte culture through hemojuvelin and BMP2/4. Blood 110(6):2182–2189
Zimmermann MB, Troesch B, Biebinger R, Egli I, Zeder C, Hurrell RF (2009) Plasma hepcidin is a modest predictor of dietary iron bioavailability in humans, whereas oral iron loading, measured by stable-isotope appearance curves, increases plasma hepcidin. Am J Clin Nutr 90(5):1280–1287
Kaundal R, Bhatia P, Arihantl J et al (2020) Randomized controlled trial of twice-daily versus alternate-day oral iron therapy in the treatment of iron-deficiency anemia. Ann Hematol 99(1):57–63
De-Regil et al (2011) Intermittent iron supplementation for improving nutrition and development in children under 12 years of age. Cochrane Database Syst Rev 2011(12):9085
Beaton George H, McCabe George P (2001) Efficacy of ıntermittent ıron supplementation in the control of ıron deficiency anaemia in developing countries. An analysıs of experience: Final report to The Micronutrient Initiative. 1999. Chapter 1. pp 1–3
Fernández-Gaxiola AC, De-Regil LM, Nasser M (2011) Intermittent iron supplementation for reducing anaemia and its associated impairments in menstruating women. Cochrane Library (12):CD009218
Smith GA, Fisher SA, Doree C, Di Angelantonio E, Roberts DJ (2014) Oral or parenteral iron supplementation to reduce deferral, iron deficiency and/or anaemia in blood donors. Cochrane Database Syst Rev (7):CD009532
Peña-Rosas JP, De-Regil LM, Dowswell T, Viteri FE (2015) Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev 2015(10):CD009997
Cook JD, Reddy MB (1995) Efficacy of weekly compared with daily iron supplementation. Am J Clin Nutr 62(1):117–120
Mehta S, Sharma BS, Gulati S, Sharma N, Goyal LK, Mehta S (2020) A Prospective, randomized, ınterventional study of oral ıron supplementation comparing daily dose with alternate day regimen using hepcidin as a biomarker in ıron deficiency anemia. J Assoc Physicians India 68(5):39–41
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaynar, L.A., Gökçen, S., Can, F. et al. Comparison of daily oral iron replacement therapy with every other day treatment in female reproductive age patients with iron-deficiency anemia. Ann Hematol 101, 1459–1464 (2022). https://doi.org/10.1007/s00277-022-04835-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-022-04835-6