Abstract
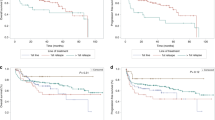
Post-transplant lymphoproliferative disorders (PTLD) exclusively affecting the central nervous system—primary CNS-PTLD (pCNS-PTLD)—are rare. There is no standard therapy, and previous case series have included heterogeneous treatment approaches. We performed a retrospective, multi-centre analysis of 14 patients with pCNS-PTLD after solid organ transplantation (SOT) treated in the prospective German PTLD registry with reduction of immunosuppression (RI), whole-brain radiotherapy (WBRT), and concurrent systemic rituximab between 2001 and 2018. Twelve of fourteen patients were kidney transplant recipients and median age at diagnosis was 65 years. Thirteen of fourteen cases (93%) were monomorphic PTLD of the diffuse large B-cell lymphoma type, and 12/13 were EBV-associated. The median dose of WBRT administered was 40 Gy with a median fraction of 2 Gy. The median number of administered doses of rituximab (375 mg/m2) IV was four. All ten patients evaluated responded to treatment (100%). Median OS was 2.5 years with a 2-year Kaplan–Meier estimate of 63% (95% confidence interval 30–83%) without any recorded relapses after a median follow-up of 2.6 years. Seven of fourteen patients (50%) suffered grade III/IV infections under therapy (fatal in two cases, 14%). During follow-up, imaging demonstrated grey matter changes interpreted as radiation toxicity in 7/10 evaluated patients (70%). The combination of RI, WBRT, and rituximab was an effective yet toxic treatment of pCNS-PTLD in this series of 14 patients. Future treatment approaches in pCNS-PTLD should take into account the significant risk of infections as well as radiation-induced neurotoxicity.

Similar content being viewed by others
Data availability
Authors elect to not share data.
References
Evens AM, Choquet S, Kroll-Desrosiers AR et al (2013) Primary CNS posttransplant lymphoproliferative disease (PTLD): an international report of 84 cases in the modern era. Am J Transplant 13:1512–1522. https://doi.org/10.1111/ajt.12211
Crane GM, Powell H, Kostadinov R et al (2015) Primary CNS lymphoproliferative disease, mycophenolate and calcineurin inhibitor usage. Oncotarget 6:33849–33866. https://doi.org/10.18632/oncotarget.5292
Dugan JP, Haverkos BM, Villagomez L et al (2018) Complete and durable responses in primary central nervous system posttransplant lymphoproliferative disorder with zidovudine, ganciclovir, rituximab, and dexamethasone. Clin Cancer Res 24:3273–3281. https://doi.org/10.1158/1078-0432.CCR-17-2685
Dharnidharka VR, Webster AC, Martinez OM et al (2016) Post-transplant lymphoproliferative disorders. Nat Rev Dis Primers 2:15088. https://doi.org/10.1038/nrdp.2015.88
Trappe R, Oertel S, Leblond V et al (2012) Sequential treatment with rituximab followed by CHOP chemotherapy in adult B-cell post-transplant lymphoproliferative disorder (PTLD): the prospective international multicentre phase 2 PTLD-1 trial. Lancet Oncol 13:196–206. https://doi.org/10.1016/S1470-2045(11)70300-X
Trappe RU, Dierickx D, Zimmermann H et al (2017) Response to rituximab induction is a predictive marker in B-cell post-transplant lymphoproliferative disorder and allows successful stratification into rituximab or R-CHOP consolidation in an international, prospective, multicenter phase II trial. J Clin Oncol 35:536–543. https://doi.org/10.1200/JCO.2016.69.3564
Cavaliere R, Petroni G, Lopes MB et al (2010) Primary central nervous system post-transplantation lymphoproliferative disorder: an International Primary Central Nervous System Lymphoma Collaborative Group Report. Cancer 116:863–870. https://doi.org/10.1002/cncr.24834
Fink SEK, Gandhi MK, Nourse JP et al (2014) A comprehensive analysis of the cellular and EBV-specific microRNAome in primary CNS PTLD identifies different patterns among EBV-associated tumors. Am J Transplant 14:2577–2587. https://doi.org/10.1111/ajt.12858
Ferreri AJM, Cwynarski K, Pulczynski E et al (2016) Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol 3:e217-227. https://doi.org/10.1016/S2352-3026(16)00036-3
Ferreri AJM, Cwynarski K, Pulczynski E et al (2017) Whole-brain radiotherapy or autologous stem-cell transplantation as consolidation strategies after high-dose methotrexate-based chemoimmunotherapy in patients with primary CNS lymphoma: results of the second randomisation of the International Extranodal Lymphoma Study Group-32 phase 2 trial. Lancet Haematol 4:e510–e523. https://doi.org/10.1016/S2352-3026(17)30174-6
Fox CP, Phillips EH, Smith J et al (2019) Guidelines for the diagnosis and management of primary central nervous system diffuse large B-cell lymphoma. Br J Haematol 184:348–363. https://doi.org/10.1111/bjh.15661
Hoang-Xuan K, Bessell E, Bromberg J et al (2015) Diagnosis and treatment of primary CNS lymphoma in immunocompetent patients: guidelines from the European Association for Neuro-Oncology. Lancet Oncol 16:e322-332. https://doi.org/10.1016/S1470-2045(15)00076-5
Zimmermann H, Trappe RU (2013) EBV and posttransplantation lymphoproliferative disease: what to do? Hematology Am Soc Hematol Educ Program 2013:95–102. https://doi.org/10.1182/asheducation-2013.1.95
Dierickx D, Tousseyn T, Gheysens O (2015) How I treat posttransplant lymphoproliferative disorders. Blood 126:2274–2283. https://doi.org/10.1182/blood-2015-05-615872
Valavoor SH, Ashraf Z, Narwal R, Ratnam S (2013) Conservative management of post-transplant central nervous system lymphoma. Int Urol Nephrol 45:1219–1222. https://doi.org/10.1007/s11255-012-0146-8
Patrick A, Wee A, Hedderman A et al (2011) High-dose intravenous rituximab for multifocal, monomorphic primary central nervous system posttransplant lymphoproliferative disorder. J Neurooncol 103:739–743. https://doi.org/10.1007/s11060-010-0425-0
Velvet AJJ, Bhutani S, Papachristos S et al (2019) A single-center experience of post-transplant lymphomas involving the central nervous system with a review of current literature. Oncotarget 10:437–448. https://doi.org/10.18632/oncotarget.26522
Bonney DK, Htwe EE, Turner A et al (2012) Sustained response to intrathecal rituximab in EBV associated post-transplant lymphoproliferative disease confined to the central nervous system following haematopoietic stem cell transplant. Pediatr Blood Cancer 58:459–461. https://doi.org/10.1002/pbc.23134
Czyzewski K, Styczynski J, Krenska A et al (2013) Intrathecal therapy with rituximab in central nervous system involvement of post-transplant lymphoproliferative disorder. Leuk Lymphoma 54:503–506. https://doi.org/10.3109/10428194.2012.718342
Swerdlow SH, Webber SA, Chadburn A, Ferry JA (2017) Post-transplant lymphoproliferative disorders. In: Swerdlow SH, Campo E, Harris NL et al (eds) WHO classification of tumours of haematopoetic and lymphoid tissues, Revised, 4th edn. International Agency for Research on Cancer, Lyon, pp 453–462
Paya CV, Fung JJ, Nalesnik MA et al (1999) Epstein-Barr virus-induced posttransplant lymphoproliferative disorders. ASTS/ASTP EBV-PTLD Task Force and The Mayo Clinic Organized International Consensus Development Meeting. Transplantation 68:1517–1525
Parker A, Bowles K, Bradley JA et al (2010) Management of post-transplant lymphoproliferative disorder in adult solid organ transplant recipients-BCSH and BTS Guidelines. Br J Haematol 149:693–705. https://doi.org/10.1111/j.1365-2141.2010.08160.x
Abrey LE, Batchelor TT, Ferreri AJM et al (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23:5034–5043. https://doi.org/10.1200/JCO.2005.13.524
Fernández-Ruiz M, López-Medrano F, Varela-Peña P et al (2012) Monitoring of immunoglobulin levels identifies kidney transplant recipients at high risk of infection. Am J Transplant 12:2763–2773. https://doi.org/10.1111/j.1600-6143.2012.04192.x
Gavrilovic IT, Hormigo A, Yahalom J et al (2006) Long-term follow-up of high-dose methotrexate-based therapy with and without whole brain irradiation for newly diagnosed primary CNS lymphoma. J Clin Oncol 24:4570–4574. https://doi.org/10.1200/JCO.2006.06.6910
Herrlinger U, Schäfer N, Fimmers R et al (2017) Early whole brain radiotherapy in primary CNS lymphoma: negative impact on quality of life in the randomized G-PCNSL-SG1 trial. J Cancer Res Clin Oncol 143:1815–1821. https://doi.org/10.1007/s00432-017-2423-5
Funding
The German PTLD registry has been supported through a grant from Roche Germany.
Author information
Authors and Affiliations
Consortia
Contributions
HZ, MN, and RUT designed the study. RUT is the principal investigator and takes primary responsibility for the paper. HZ, MN, CP, PR, NB, RMH, IAH, DH, MR, and RUT recruited and treated significant numbers of patients. HZ, MN, and RUT collected, analyzed, and interpreted the data. CP performed, analyzed, and collated radiology studies. MR performed reference flow cytometry. WK and IA performed reference haematopathology. HZ, MN, and RUT wrote the paper. All authors had full access to the final version of the manuscript and agreed to publication.
Corresponding author
Ethics declarations
Ethics approval
The German PTLD registry was approved by the appropriate Ethics committees.
Consent to participate
Patients provided informed consent to the German PTLD registry according to the Declaration of Helsinki.
Conflict of interest
Dr. Zimmermann reports institutional grants from Atara and Roche, and travel support from Atara, Celgene, and Jansen, outside the submitted work. Dr. Hauser reports personal fees or travel support from Astellas, Biotest, Hexal, Neovii, Novartis, and Roche, all outside the submitted work. Dr. Ritgen reports personal fees from Hoffman LaRoche, AbbVie, AstraZeneca, and Jansen, all outside the submitted work. Claudia Pietschmann reports travel support by KS Pharma, outside the submitted work. Dr. Trappe reports institutional grants from Atara and Roche and non-financial support from Roche, Atara, Celgene, Janssen, and AbbVie, all outside the submitted work. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zimmermann, H., Nitsche, M., Pott, C. et al. Reduction of immunosuppression combined with whole-brain radiotherapy and concurrent systemic rituximab is an effective yet toxic treatment of primary central nervous system post-transplant lymphoproliferative disorder (pCNS-PTLD): 14 cases from the prospective German PTLD registry. Ann Hematol 100, 2043–2050 (2021). https://doi.org/10.1007/s00277-021-04548-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-021-04548-2