Abstract
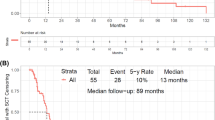
The prognosis of 11q23/KMT2A-rearranged (KMT2A-r) acute leukemia (AL) after allogeneic hematopoietic stem cell transplantation (allo-HSCT) is poor. Minimal residual disease (MRD) is an important prognostic factor for relapse. Thus, we aimed to identify the evolution of KMT2A before and after allo-HSCT and the efficacy of preemptive immunotherapies for KMT2A-r AL patients receiving allo-HSCT. KMT2A expression was determined through TaqMan-based RQ-PCR technology. Preemptive immunotherapies included interferon-α and donor lymphocyte infusion. We collected 1751 bone marrow samples from 177 consecutive KMT2A-r AL patients. Pre-HSCT KMT2A positivity was correlated with post-HSCT KMT2A positivity (correlation coefficient=0.371, P<0.001). The rates of achieving KMT2A negativity after allo-HSCT were 96.6%, 92.9%, and 68.8% in the pre-HSCT low-level group (>0, <0.1%), intermediate-level group (≥ 0.1%, <1%), and high-level group (≥1%), respectively. The rates of regaining KMT2A positivity after allo-HSCT were 7.7%, 35.7%, 38.5%, and 45.5% for the pre-HSCT KMT2A-negative, low-level, intermediate-level, and high-level groups, respectively (P<0.001). The 4-year cumulative incidence of relapse after allo-HSCT was as high as 53.7% in the pre-HSCT KMT2A expression ≥ 0.1% group, which was compared to the KMT2A-negative group (15.1%) and KMT2A <0.1% group (31.2%). The clinical outcomes of patients with post-HSCT KMT2A positivity were poorer than those of patients with persistent KMT2A negativity. Although post-HSCT preemptive immunotherapies might help to achieve KMT2A negativity, the long-term efficacy was unsatisfactory. Thus, pre-HSCT KMT2A positivity was significantly associated with post-HSCT KMT2A positivity. The clinical outcomes of patients with post-HSCT KMT2A positivity were poor, which might not be overcome by commonly used immunotherapies.





Similar content being viewed by others
References
Schoch C, Schnittger S, Klaus M, Kern W, Hiddemann W, Haferlach T (2003) AML with 11q23/MLL abnormalities as defined by the WHO classification: incidence, partner chromosomes, FAB subtype, age distribution, and prognostic impact in an unselected series of 1897 cytogenetically analyzed AML cases. Blood 102(7):2395–2402. https://doi.org/10.1182/blood-2003-02-0434
Pui CH, Chessells JM, Camitta B, Baruchel A, Biondi A, Boyett JM, Carroll A, Eden OB, Evans WE, Gadner H, Harbott J, Harms DO, Harrison CJ, Harrison PL, Heerema N, Janka-Schaub G, Kamps W, Masera G, Pullen J, Raimondi SC, Richards S, Riehm H, Sallan S, Sather H, Shuster J, Silverman LB, Valsecchi MG, Vilmer E, Zhou Y, Gaynon PS, Schrappe M (2003) Clinical heterogeneity in childhood acute lymphoblastic leukemia with 11q23 rearrangements. Leukemia 17(4):700–706. https://doi.org/10.1038/sj.leu.2402883
Meyer C, Burmeister T, Groger D, Tsaur G, Fechina L, Renneville A, Sutton R, Venn NC, Emerenciano M, Pombo-de-Oliveira MS, Barbieri Blunck C, Almeida Lopes B, Zuna J, Trka J, Ballerini P, Lapillonne H, De Braekeleer M, Cazzaniga G, Corral Abascal L, van der Velden VHJ, Delabesse E, Park TS, Oh SH, Silva MLM, Lund-Aho T, Juvonen V, Moore AS, Heidenreich O, Vormoor J, Zerkalenkova E, Olshanskaya Y, Bueno C, Menendez P, Teigler-Schlegel A, Zur Stadt U, Lentes J, Gohring G, Kustanovich A, Aleinikova O, Schafer BW, Kubetzko S, Madsen HO, Gruhn B, Duarte X, Gameiro P, Lippert E, Bidet A, Cayuela JM, Clappier E, Alonso CN, Zwaan CM, van den Heuvel-Eibrink MM, Izraeli S, Trakhtenbrot L, Archer P, Hancock J, Moricke A, Alten J, Schrappe M, Stanulla M, Strehl S, Attarbaschi A, Dworzak M, Haas OA, Panzer-Grumayer R, Sedek L, Szczepanski T, Caye A, Suarez L, Cave H, Marschalek R (2018) The MLL recombinome of acute leukemias in 2017. Leukemia 32:273–284. https://doi.org/10.1038/leu.2017.213
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, Levine RL, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz M, Sierra J, Tallman MS, Tien HF, Wei AH, Lowenberg B, Bloomfield CD (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129(4):424–447. https://doi.org/10.1182/blood-2016-08-733196
Mancini M, Scappaticci D, Cimino G, Nanni M, Derme V, Elia L, Tafuri A, Vignetti M, Vitale A, Cuneo A, Castoldi G, Saglio G, Pane F, Mecucci C, Camera A, Specchia G, Tedeschi A, Di Raimondo F, Fioritoni G, Fabbiano F, Marmont F, Ferrara F, Cascavilla N, Todeschini G, Nobile F, Kropp MG, Leoni P, Tabilio A, Luppi M, Annino L, Mandelli F, Foa R (2005) A comprehensive genetic classification of adult acute lymphoblastic leukemia (ALL): analysis of the GIMEMA 0496 protocol. Blood 105(9):3434–3441. https://doi.org/10.1182/blood-2004-07-2922
Moorman AV, Harrison CJ, Buck GA, Richards SM, Secker-Walker LM, Martineau M, Vance GH, Cherry AM, Higgins RR, Fielding AK, Foroni L, Paietta E, Tallman MS, Litzow MR, Wiernik PH, Rowe JM, Goldstone AH, Dewald GW (2007) Karyotype is an independent prognostic factor in adult acute lymphoblastic leukemia (ALL): analysis of cytogenetic data from patients treated on the Medical Research Council (MRC) UKALLXII/Eastern Cooperative Oncology Group (ECOG) 2993 trial. Blood 109(8):3189–3197. https://doi.org/10.1182/blood-2006-10-051912
Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, Pettenati MJ, Patil SR, Rao KW, Watson MS, Koduru PR, Moore JO, Stone RM, Mayer RJ, Feldman EJ, Davey FR, Schiffer CA, Larson RA, Bloomfield CD, Cancer, Leukemia Group B (2002) Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 100(13):4325–4336. https://doi.org/10.1182/blood-2002-03-0772
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A (1998) The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood 92(7):2322–2333
Grimwade D, Walker H, Harrison G, Oliver F, Chatters S, Harrison CJ, Wheatley K, Burnett AK, Goldstone AH (2001) The predictive value of hierarchical cytogenetic classification in older adults with acute myeloid leukemia (AML): analysis of 1065 patients entered into the United Kingdom Medical Research Council AML11 trial. Blood 98(5):1312–1320. https://doi.org/10.1182/blood.v98.5.1312
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, Paietta E, Willman CL, Head DR, Rowe JM, Forman SJ, Appelbaum FR (2000) Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 96(13):4075–4083
Xu L, Chen H, Chen J, Han M, Huang H, Lai Y, Liu D, Liu Q, Liu T, Jiang M, Ren H, Song Y, Sun Z, Wang J, Wu D, Zhou D, Zou P, Liu K, Huang X (2018) The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China-recommendations from the Chinese Society of Hematology. J Hematol Oncol 11(1):33. https://doi.org/10.1186/s13045-018-0564-x
Lv M, Chang Y, Huang X (2019) Everyone has a donor: contribution of the Chinese experience to global practice of haploidentical hematopoietic stem cell transplantation. Front Med 13(1):45–56. https://doi.org/10.1007/s11684-017-0595-7
Wang Y, Liu QF, Qin YZ, Liu DH, Xu LP, Jiang B, Jiang Q, Dai M, Yu SJ, Jiang XM, Liu YR, Huang XJ (2014) Improved outcome with hematopoietic stem cell transplantation in a poor prognostic subgroup of patients with mixed-lineage-leukemia-rearranged acute leukemia: Results from a prospective, multi-center study. Am J Hematol 89(2):130–136. https://doi.org/10.1002/ajh.23595
Mo XD, Tang BL, Zhang XH, Zheng CC, Xu LP, Zhu XY, Wang Y, Liu HL, Yan CH, Chu XD, Chen H, Geng LQ, Liu KY, Sun ZM, Huang XJ (2016) Comparison of outcomes after umbilical cord blood and unmanipulated haploidentical hematopoietic stem cell transplantation in children with high-risk acute lymphoblastic leukemia. Int J Cancer 139(9):2106–2115. https://doi.org/10.1002/ijc.30249
Mo XD, Xu LP, Zhang XH, Liu DH, Wang Y, Chen H, Yan CH, Chen YH, Han W, Wang FR, Wang JZ, Liu KY, Huang XJ (2015) Haploidentical hematopoietic stem cell transplantation in adults with Philadelphia-negative acute lymphoblastic leukemia: no difference in the high- and low-risk groups. Int J Cancer 136(7):1697–1707. https://doi.org/10.1002/ijc.29146
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, Fan ZP, Wu DP, Huang XJ (2015) Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood 125(25):3956–3962. https://doi.org/10.1182/blood-2015-02-627786
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, Wu MQ, Wu DP, Huang XJ (2016) Haploidentical versus matched-sibling transplant in adults with Philadelphia-negative high-risk acute lymphoblastic leukemia: a biologically phase III randomized study. Clin Cancer Res 22(14):3467–3476. https://doi.org/10.1158/1078-0432.Ccr-15-2335
Mo XD, Lv M, Huang XJ (2017) Preventing relapse after haematopoietic stem cell transplantation for acute leukaemia: the role of post-transplantation minimal residual disease (MRD) monitoring and MRD-directed intervention. Br J Haematol 179(2):184–197. https://doi.org/10.1111/bjh.14778
Wang Y, Chen H, Chen J, Han M, Hu J, Jiong H, Huang H, Lai Y, Liu D, Liu Q, Liu T, Jiang M, Ren H, Song Y, Sun Z, Wang C, Wang J, Wu D, Xu K, Zhang X, Xu L, Liu K, Huang X (2018) The consensus on the monitoring, treatment, and prevention of leukemia relapse after allogeneic hematopoietic stem cell transplantation in China. Cancer Lett 438:63–75. https://doi.org/10.1016/j.canlet.2018.08.030
Liu J, Wang Y, Xu LP, Liu DH, Qin YZ, Chang YJ, Liu KY, Huang XJ (2014) Monitoring mixed lineage leukemia expression may help identify patients with mixed lineage leukemia--rearranged acute leukemia who are at high risk of relapse after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 20(7):929–936. https://doi.org/10.1016/j.bbmt.2014.03.008
Dominietto A, Pozzi S, Miglino M, Albarracin F, Piaggio G, Bertolotti F, Grasso R, Zupo S, Raiola AM, Gobbi M, Frassoni F, Bacigalupo A (2007) Donor lymphocyte infusions for the treatment of minimal residual disease in acute leukemia. Blood 109(11):5063–5064. https://doi.org/10.1182/blood-2007-02-072470
Yan CH, Liu DH, Liu KY, Xu LP, Liu YR, Chen H, Han W, Wang Y, Qin YZ, Huang XJ (2012) Risk stratification-directed donor lymphocyte infusion could reduce relapse of standard-risk acute leukemia patients after allogeneic hematopoietic stem cell transplantation. Blood 119(14):3256–3262. https://doi.org/10.1182/blood-2011-09-380386
Mo XD, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, Chen YH, Han W, Wang FR, Wang JZ, Liu KY, Huang XJ (2016) Salvage chemotherapy followed by granulocyte colony-stimulating factor-primed donor leukocyte infusion with graft-vs.-host disease control for minimal residual disease in acute leukemia/myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation: prognostic factors and clinical outcomes. Eur J Haematol 96(3):297–308. https://doi.org/10.1111/ejh.12591
Mo XD, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, Chen YH, Han W, Wang FR, Wang JZ, Liu KY, Huang XJ (2017) Comparison of outcomes after donor lymphocyte infusion with or without prior chemotherapy for minimal residual disease in acute leukemia/myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation. Ann Hematol 96(5):829–838. https://doi.org/10.1007/s00277-017-2960-7
Mo XD, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, Chen YH, Han W, Wang FR, Wang JZ, Liu KY, Huang XJ (2015) Interferon-alpha: a potentially effective treatment for minimal residual disease in acute leukemia/myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 21(11):1939–1947. https://doi.org/10.1016/j.bbmt.2015.06.014
Mo XD, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, Chen YH, Han W, Wang FR, Wang JZ, Liu KY, Huang XJ (2017) IFN-alpha is effective for treatment of minimal residual disease in patients with acute leukemia after allogeneic hematopoietic stem cell transplantation: results of a registry study. Biol Blood Marrow Transplant 23(8):1303–1310. https://doi.org/10.1016/j.bbmt.2017.04.023
Mo XD, Wang Y, Zhang XH, Xu LP, Yan CH, Chen H, Chen YH, Qin YZ, Liu KY, Huang XJ (2018) Interferon-alpha is effective for treatment of minimal residual disease in patients with t(8;21) acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation: results of a prospective registry study. Oncologist 23(11):1349–1357. https://doi.org/10.1634/theoncologist.2017-0692
Mo X, Zhang X, Xu L, Wang Y, Yan C, Chen H, Chen Y, Han W, Wang F, Wang J, Liu K, Huang X (2019) Minimal residual disease-directed immunotherapy for high-risk myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation. Front Med 13(3):354–364. https://doi.org/10.1007/s11684-018-0665-5
Huang XJ, Xu LP, Liu KY, Liu DH, Wang Y, Chen H, Chen YH, Han W, Wang JZ, Chen Y, Zhang XH, Shi HX, Wang FR, Tang FF (2009) Partially matched related donor transplantation can achieve outcomes comparable with unrelated donor transplantation for patients with hematologic malignancies. Clin Cancer Res 15(14):4777–4783. https://doi.org/10.1158/1078-0432.Ccr-09-0691
Wang Y, Wu DP, Liu QF, Xu LP, Liu KY, Zhang XH, Yu WJ, Xu Y, Huang F, Huang XJ (2019) Low-dose post-transplant cyclophosphamide and anti-thymocyte globulin as an effective strategy for GVHD prevention in haploidentical patients. J Hematol Oncol 12(1):88. https://doi.org/10.1186/s13045-019-0781-y
Wang Y, Chang YJ, Xu LP, Liu KY, Liu DH, Zhang XH, Chen H, Han W, Chen YH, Wang FR, Wang JZ, Chen Y, Yan CH, Huo MR, Li D, Huang XJ (2014) Who is the best donor for a related HLA haplotype-mismatched transplant? Blood 124(6):843–850. https://doi.org/10.1182/blood-2014-03-563130
Mo XD, Zhang YY, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, Chen YH, Chang YJ, Liu KY, Huang XJ (2018) The role of collateral related donors in haploidentical hematopoietic stem cell transplantation. Sci Bull 63(20):1376–1382. https://doi.org/10.1016/j.scib.2018.08.008
Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, Chen YH, Wang JZ, Gao ZY, Zhang YC, Jiang Q, Shi HX, Lu DP (2006) Haploidentical hematopoietic stem cell transplantation without in vitro T-cell depletion for the treatment of hematological malignancies. Bone Marrow Transplant 38(4):291–297. https://doi.org/10.1038/sj.bmt.1705445
Liu SN, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, Chen YH, Han W, Wang FR, Wang JZ, Liu KY, Huang XJ, Mo XD (2020) Prognostic factors and long-term follow-up of basiliximab for steroid-refractory acute graft-versus-host disease: Updated experience from a large-scale study. Am J Hematol 95:927–936. https://doi.org/10.1002/ajh.25839
Zhao XS, Liu YR, Zhu HH, Xu LP, Liu DH, Liu KY, Huang XJ (2012) Monitoring MRD with flow cytometry: an effective method to predict relapse for ALL patients after allogeneic hematopoietic stem cell transplantation. Ann Hematol 91(2):183–192. https://doi.org/10.1007/s00277-011-1285-1
Chang YJ, Wang Y, Liu YR, Xu LP, Zhang XH, Chen H, Chen YH, Wang FR, Han W, Sun YQ, Yan CH, Tang FF, Mo XD, Liu KY, Huang XJ (2017) Haploidentical allograft is superior to matched sibling donor allograft in eradicating pre-transplantation minimal residual disease of AML patients as determined by multiparameter flow cytometry: a retrospective and prospective analysis. J Hematol Oncol 10(1):134. https://doi.org/10.1186/s13045-017-0502-3
Zhao XS, Liu YR, Xu LP, Wang Y, Zhang XH, Chen H, Chen YH, Han W, Sun YQ, Yan CH, Mo XD, Wang YZ, Fan QZ, Wang XY, Liu KY, Huang XJ, Chang YJ (2019) Minimal residual disease status determined by multiparametric flow cytometry pretransplantation predicts the outcome of patients with ALL receiving unmanipulated haploidentical allografts. Am J Hematol 94(5):512–521. https://doi.org/10.1002/ajh.25417
Zhao XS, Jin S, Zhu HH, Xu LP, Liu DH, Chen H, Liu KY, Huang XJ (2012) Wilms’ tumor gene 1 expression: an independent acute leukemia prognostic indicator following allogeneic hematopoietic SCT. Bone Marrow Transplant 47(4):499–507. https://doi.org/10.1038/bmt.2011.121
Gooley TA, Leisenring W, Crowley J, Storer BE (1999) Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 18(6):695–706. https://doi.org/10.1002/(sici)1097-0258(19990330)18:6<695::aid-sim60>3.0.co;2-o
Konuma T, Mizuno S, Kondo T, Yamaguchi H, Fukuda T, Uchida N, Najima Y, Kanamori H, Ota S, Nakamae H, Nakamae M, Mizuno I, Sugita J, Onishi Y, Yokota A, Takahashi S, Kanda Y, Ichinohe T, Atsuta Y, Yano S (2018) Allogeneic hematopoietic cell transplantation in adult acute myeloid leukemia with 11q23 abnormality: a retrospective study of the Adult Acute Myeloid Leukemia Working Group of the Japan Society for Hematopoietic Cell Transplantation (JSHCT). Ann Hematol 97(11):2173–2183. https://doi.org/10.1007/s00277-018-3419-1
Hong M, Wu Q, Hu C, Fang J, You Y, Zhong Z, Zou P, Hu Y, Xia L (2012) Idarubicin-intensified BUCY2 regimens may lower relapse rate and improve survival in patients undergoing allo-SCT for high-risk hematological malignancies: a retrospective analysis. Bone Marrow Transplant 47(2):196–202. https://doi.org/10.1038/bmt.2011.66
Tang W, Fan X, Wang L, Hu J (2015) Busulfan and fludarabine conditioning regimen given at hematological nadir of cytoreduction fludarabine, cytarabine, and idarubicin chemotherapy in patients with refractory acute myeloid leukemia undergoing allogeneic stem cell transplantation: a single arm pilot consort study. Medicine 94(15):e706. https://doi.org/10.1097/md.0000000000000706
Andersson BS, Valdez BC, de Lima M, Wang X, Thall PF, Worth LL, Popat U, Madden T, Hosing C, Alousi A, Rondon G, Kebriaei P, Shpall EJ, Jones RB, Champlin RE (2011) Clofarabine +/- fludarabine with once daily i.v. busulfan as pretransplant conditioning therapy for advanced myeloid leukemia and MDS. Biol Blood Marrow Transplant 17(6):893–900. https://doi.org/10.1016/j.bbmt.2010.09.022
Farag SS, Wood LL, Schwartz JE, Srivastava S, Nelson RP Jr, Robertson MJ, Abonour R, Secrest A, Cox E, Baute J, Sullivan C, Kane K, Jones DR (2011) Phase I trial and pharmacokinetic study of high-dose clofarabine and busulfan and allogeneic stem cell transplantation in adults with high-risk and refractory acute leukemia. Leukemia 25(4):599–605. https://doi.org/10.1038/leu.2010.319
Nemecek ER, Guthrie KA, Sorror ML, Wood BL, Doney KC, Hilger RA, Scott BL, Kovacsovics TJ, Maziarz RT, Woolfrey AE, Bedalov A, Sanders JE, Pagel JM, Sickle EJ, Witherspoon R, Flowers ME, Appelbaum FR, Deeg HJ (2011) Conditioning with treosulfan and fludarabine followed by allogeneic hematopoietic cell transplantation for high-risk hematologic malignancies. Biol Blood Marrow Transplant 17(3):341–350. https://doi.org/10.1016/j.bbmt.2010.05.007
Cieri N, Greco R, Crucitti L, Morelli M, Giglio F, Levati G, Assanelli A, Carrabba MG, Bellio L, Milani R, Lorentino F, Stanghellini MT, De Freitas T, Marktel S, Bernardi M, Corti C, Vago L, Bonini C, Ciceri F, Peccatori J (2015) Post-transplantation cyclophosphamide and sirolimus after haploidentical hematopoietic stem cell transplantation using a treosulfan-based myeloablative conditioning and peripheral blood stem cells. Biol Blood Marrow Transplant 21(8):1506–1514. https://doi.org/10.1016/j.bbmt.2015.04.025
Wang Y, Liu DH, Xu LP, Liu KY, Chen H, Zhang XH, Chen YH, Han W, Wang FR, Wang JZ, Yan CH, Huang XJ (2012) Prevention of relapse using granulocyte CSF-primed PBPCs following HLA-mismatched/haploidentical, T-cell-replete hematopoietic SCT in patients with advanced-stage acute leukemia: a retrospective risk-factor analysis. Bone Marrow Transplant 47(8):1099–1104. https://doi.org/10.1038/bmt.2011.213
Wang Y, Liu DH, Fan ZP, Sun J, Wu XJ, Ma X, Xu LP, Liu KY, Liu QF, Wu DP, Huang XJ (2012) Prevention of relapse using DLI can increase survival following HLA-identical transplantation in patients with advanced-stage acute leukemia: a multi-center study. Clin Transpl 26(4):635–643. https://doi.org/10.1111/j.1399-0012.2012.01626.x
Mo X, Zhao X, Xu L, Liu D, Zhang X, Chen H, Wang Y, Huang X (2014) Interferon alpha: the salvage therapy for patients with unsatisfactory response to minimal residual disease-directed modified donor lymphocyte infusion. Chin Med J 127(14):2583–2587
Mo X, Zhang X, Xu L, Wang Y, Yan C, Chen H, Chen Y, Han W, Wang F, Wang J, Liu K, Huang X (2019) Interferon-alpha salvage treatment is effective for patients with acute leukemia/myelodysplastic syndrome with unsatisfactory response to minimal residual disease-directed donor lymphocyte infusion after allogeneic hematopoietic stem cell transplantation. Front Med 13(2):238–249. https://doi.org/10.1007/s11684-017-0599-3
Stein EM, Garcia-Manero G, Rizzieri DA, Tibes R, Berdeja JG, Savona MR, Jongen-Lavrenic M, Altman JK, Thomson B, Blakemore SJ, Daigle SR, Waters NJ, Suttle AB, Clawson A, Pollock R, Krivtsov A, Armstrong SA, DiMartino J, Hedrick E, Lowenberg B, Tallman MS (2018) The DOT1L inhibitor pinometostat reduces H3K79 methylation and has modest clinical activity in adult acute leukemia. Blood 131(24):2661–2669. https://doi.org/10.1182/blood-2017-12-818948
Steinhilber D, Marschalek R (2018) How to effectively treat acute leukemia patients bearing MLL-rearrangements ? Biochem Pharmacol 147:183–190. https://doi.org/10.1016/j.bcp.2017.09.007
Platzbecker U, Wermke M, Radke J, Oelschlaegel U, Seltmann F, Kiani A, Klut IM, Knoth H, Rollig C, Schetelig J, Mohr B, Graehlert X, Ehninger G, Bornhauser M, Thiede C (2012) Azacitidine for treatment of imminent relapse in MDS or AML patients after allogeneic HSCT: results of the RELAZA trial. Leukemia 26(3):381–389. https://doi.org/10.1038/leu.2011.234
Shah NN, Fry TJ (2019) Mechanisms of resistance to CAR T cell therapy. Nat Rev Clin Oncol 16(6):372–385. https://doi.org/10.1038/s41571-019-0184-6
Balgobind BV, Raimondi SC, Harbott J, Zimmermann M, Alonzo TA, Auvrignon A, Beverloo HB, Chang M, Creutzig U, Dworzak MN, Forestier E, Gibson B, Hasle H, Harrison CJ, Heerema NA, Kaspers GJ, Leszl A, Litvinko N, Nigro LL, Morimoto A, Perot C, Pieters R, Reinhardt D, Rubnitz JE, Smith FO, Stary J, Stasevich I, Strehl S, Taga T, Tomizawa D, Webb D, Zemanova Z, Zwaan CM, van den Heuvel-Eibrink MM (2009) Novel prognostic subgroups in childhood 11q23/MLL-rearranged acute myeloid leukemia: results of an international retrospective study. Blood 114(12):2489–2496. https://doi.org/10.1182/blood-2009-04-215152
Inaba H, Zhou Y, Abla O, Adachi S, Auvrignon A, Beverloo HB, de Bont E, Chang TT, Creutzig U, Dworzak M, Elitzur S, Fynn A, Forestier E, Hasle H, Liang DC, Lee V, Locatelli F, Masetti R, De Moerloose B, Reinhardt D, Rodriguez L, Van Roy N, Shen S, Taga T, Tomizawa D, Yeoh AE, Zimmermann M, Raimondi SC (2015) Heterogeneous cytogenetic subgroups and outcomes in childhood acute megakaryoblastic leukemia: a retrospective international study. Blood 126(13):1575–1584. https://doi.org/10.1182/blood-2015-02-629204
Pigneux A, Labopin M, Maertens J, Cordonnier C, Volin L, Socie G, Blaise D, Craddock C, Milpied N, Bacher U, Malard F, Esteve J, Nagler A, Mohty M, Acute Leukemia Working Party E (2015) Outcome of allogeneic hematopoietic stem-cell transplantation for adult patients with AML and 11q23/MLL rearrangement (MLL-r AML). Leukemia 29(12):2375–2381. https://doi.org/10.1038/leu.2015.143
Funding
This work was supported by grants from the Capital’s Funds for Health Improvement and Research (2018-4-4089), Peking University Medicine Fund of Fostering Young Scholars’ Scientific & Technological Innovation (BMU2020PY007), the Key Program of the National Natural Science Foundation of China (81930004), the National Key Research and Development Program of China (2017YFA0104500), the National Natural Science Foundation of China (81670175, 81870137 and 81900173), Innovative Research Groups of the National Natural Science Foundation of China (81621001), and CAMS Innovation Fund for Medical Sciences (CIFMS) (2019-I2M-5-034), and the Fundamental Research Funds for the Central Universities.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Statement
Informed consent was obtained from all patients for being included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, J., Zhang, XH., Xu, LP. et al. Minimal residual disease monitoring and preemptive immunotherapies for frequent 11q23 rearranged acute leukemia after allogeneic hematopoietic stem cell transplantation. Ann Hematol 100, 1267–1281 (2021). https://doi.org/10.1007/s00277-021-04488-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-021-04488-x