Abstract
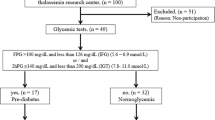
The use of cardiac and hepatic T2* MRI measurements to predict the amount of iron accumulation in these organs has been studied extensively and was suggested to be used reliably. However, it may not be practical to screen other organs with MRI related to economical issues and also the prolonged imaging durations. Herein, we aimed to test the use of fasting glucose, fasting, and postprandial insulin, homeostasis model assessment-insulin resistance (HOMA-IR) (calculated as insulin (μIU/ml) × glucose (mg/dl)/22.5), and homeostasis model assessment B score (HOMA-B) (calculated as insulin (μIU/ml) × 20/glucose (mg/dl) − 3.5) to estimate the tissue iron measured with MRI. A total of 37 patients with β-thalassemia major (BTM), age 20.8 ± 6.3 years (7.1–36.8), were enrolled. MRI measurements were done concomitantly to the biochemical tests for glucose metabolism. A positive correlation between HOMA-IR and hepatic iron loading and a negative correlation between pancreatic T2* and fasting blood glucose were found. A positive correlation was found between fasting insulin levels and pancreatic R2* measures. Additionally, a correlation was detected between cardiac and pancreatic iron accumulations. In centers where T2*/R2* MRI facilities are unavailable, fasting insulin, fasting glucose, and HOMA-IR measurements may be used to predict iron overload and may urge the physician for MRI assessment in case of a deterioration in these biochemical tests. Since hepatic iron loading correlated with insulin resistance development, the insulin resistance among patients with BTM may partially be explained with decreased hepatic insulin clearance from heavily iron-loaded liver.

Similar content being viewed by others
References
Cappellini MD, Cohen A, Eleftheriou A, Piga A, Porter J, Taher A (2008) Guidelines for the clinical management of thalassaemia, 2nd edn. Thalassaemia International Federation, Nicosia
Cunningham MJ, Sankaran VG, Nathan DG, Orkin SH (2009) The Thalassemias. In: Nathan DG, Orkin SH (eds) Nathan and Oski’s hematology of infancy and childhood, 7th edn. WB Saunders, Philadelphia, pp 1015–1106
Li MJ, Peng SS, Lu MY, Chang HH, Yang YL, Jou ST, Lin DT, Lin KH (2014) Diabetes mellitus in patients with thalassemia major. Pediatr Blood Cancer 61:20–24. doi:10.1002/pbc.24754
Cario H, Holl RW, Debatin KM, Kohne E (2003) Insulin sensitivity and beta-cell secretion in thalassaemia major with secondary haemochromatosis: assessment by oral glucose tolerance test. Eur J Pediatr 162:139–146
De Assis RA, Ribeiro AA, Kay FU, Rosemberg LA, Nomura CH, Loggetto SR, Araujo AS, Fabron Junior A, de Almeida Veríssimo MP, Baldanzi GR, Espósito BP, Baroni RH, Wood JC, Hamerschlak N (2012) Pancreatic iron stores assessed by magnetic resonance imaging (MRI) in beta thalassemic patients. Eur J Radiol 81:1465–1470. doi:10.1016/j.ejrad.2011.03.077
Cavallo-Perin P, Pacini G, Cerutti F, Bessone A, Condo C, Sacchetti L, Piga A, Pagano G (1995) Insulin resistance and hyperinsulinemia in homozygous beta-thalassemia. Metabolism 44:281–286
Kohgo Y, Ikuta K, Ohtake T, Torimoto Y, Kato J (2007) Iron overload and cofactors with special reference to alcohol, hepatitis C virus infection and steatosis/insulin resistance. World J Gastroenterol 21:4699–4706
Platis O, Anagnostopoulos G, Farmaki K, Posantzis M, Gotsis E, Tolis G (2004) Glucose metabolism disorders improvement in patients with thalassaemia major after 24–36 months of intensive chelation therapy. Pediatr Endocrinol Rev 2:279–281
Au WY, Lam WW, Chu W, Tam S, Wong WK, Liang R, Ha SY (2008) A T2* magnetic resonance imaging study of pancreatic iron overload in thalassemia major. Haematologica 93:116–119. doi:10.3324/haematol.11768
Ooi GC, Khong PL, Chan GC, Chan KN, Chan KL, Lam W, Ng I, Ha SY (2004) Magnetic resonance screening of iron status in transfusion-dependent beta-thalassaemia patients. Br J Haematol 124:385–390
Noetzli LJ, Papudesi J, Coates TD, Wood JC (2009) Pancreatic iron loading predicts cardiac iron loading in thalassemia major. Blood 114:4021–4026. doi:10.1182/blood-2009-06-225615
Barlow SE (2007) Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120:164–192
CDC, “National health and nutrition examination survey: anthropometry procedures manual,” August 2014, http://www.cdc.gov/nchs/data/nhanes/nhanes1112/AnthropometryProceduresManual.pdf
Angelucci E, Brittenham GM, McLaren CE, Ripalti M, Baronciani D, Giardini C, Galimberti M, Polchi P, Lucarelli G (2000) Hepatic iron concentration and total body iron stores in thalassemia major. N Engl J Med 343:327–331
Lam WW, Au WY, Chu WC, Tam S, Ha SY, Pennell DJ (2008) One-stop measurement of iron deposition in the anterior pituitary, liver, and heart in thalassemia patients. J Magn Reson Imaging 28:29–33. doi:10.1002/jmri.21433
Noetzli LJ, Panigrahy A, Mittelman SD, Hyderi A, Dongelyan A, Coates TD, Wood JC (2012) Pituitary iron and volume predict hypogonadism in transfusional iron overload. Am J Hematol 87:167–171. doi:10.1002/ajh.22247
Borgna-Pignatti C, Meloni A, Guerrini G, Gulino L, Filosa A, Ruffo GB, Casini T, Chiodi E, Lombardi M, Pepe A (2014) Myocardial iron overload in thalassaemia major. How early to check? Br J Haematol 164:579–585. doi:10.1111/bjh.12643
Yang G, Liu R, Peng P, Long L, Zhang X, Yang W, Tan S, Pan H, Long X, He T, Anderson L, Lai Y (2014) How early can myocardial iron overload occur in beta thalassemia major? PLoS One 9:e85379. doi:10.1371/journal.pone.0085379
Acknowledgments
All of the authors namely Munevver Bas, Fatma Gumruk, Nazlı Gonc, Mualla Cetin, Murat Tuncer, Tuncay Hazırolan, Gokce Yildirim, Erdem Karabulut, and Sule Unal contributed equally in the research design, acquisition, analysis, or interpretation of data. The study has not been financially supported.
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bas, M., Gumruk, F., Gonc, N. et al. Biochemical markers of glucose metabolism may be used to estimate the degree and progression of iron overload in the liver and pancreas of patients with β-thalassemia major. Ann Hematol 94, 1099–1104 (2015). https://doi.org/10.1007/s00277-015-2342-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2342-y