Abstract
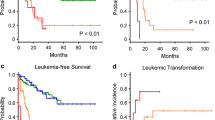
To better understand the predictive factors and improve clinical outcome of allogeneic transplant for patients with myelodysplastic syndrome (MDS), we retrospectively analyzed the post-transplant outcome of 60 Southeast Asian patients with MDS. Multivariate analysis showed that WHO classification-based Prognostic Scoring System (WPSS) significantly affect overall survival (OS), progression-free survival (PFS), cumulative incidence of relapse (CIR), and cumulative incidence of non-relapse mortality (CINRM). Stratified by WPSS into very low/low, intermediate, high, and very high-risk categories, 3-year OS was 100, 61, 37, and 18 % (p = 0.02); PFS was 100, 55, 32, and 18 % (p = 0.014); CIR was 12, 24, 38, and 59 % (p = 0.024); CINRM was 0, 6, 12, and 26 % (p = 0.037), respectively. WHO classification, Revised International Prognostic Scoring System (IPSS-R), IPSS-R-defined cytogenetic risk groups, donor gender, and acute and chronic graft vs host disease (GVHD) also influenced different aspects of transplant outcome. We found that WPSS is a powerful predictor of post-transplant outcome. WPSS provides an important model not only for prognostication but also for exploration of further post-transplant measures such as immunological maneuvers or novel therapy to improve the poor outcome of high-risk patients.


Similar content being viewed by others
References
Cazzola M, Malcovati L (2005) Myelodysplastic syndromes—coping with ineffective hematopoiesis. N Engl J Med 352:536–538
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A et al (2009) The 2008 revision of the world health organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114:937–951
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al (1997) International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 89:2079–2088
Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R et al (2007) Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol 25:3503–3510
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F et al (2012) Revised international prognostic scoring system for myelodysplastic syndromes. Blood 120:2454–2465
Garcia-Manero G (2014) Myelodysplastic syndromes: 2014 update on diagnosis, risk-stratification, and management. Am J Hematol 89:97–108
Deeg HJ, Shulman HM, Anderson JE, Bryant EM, Gooley TA, Slattery JT et al (2000) Allogeneic and syngeneic marrow transplantation for myelodysplastic syndrome in patients 55 to 66 years of age. Blood 95:1188–1194
Sierra J, Pérez WS, Rozman C, Carreras E, Klein JP, Rizzo JD et al (2002) Bone marrow transplantation from HLA-identical siblings as treatment for myelodysplasia. Blood 100:1997–2004
de Lima M, Anagnostopoulos A, Munsell M, Shahjahan M, Ueno N, Ippoliti C et al (2004) Nonablative versus reduced-intensity conditioning regimens in the treatment of acute myeloid leukemia and high-risk myelodysplastic syndrome: dose is relevant for long-term disease control after allogeneic hematopoietic stem cell transplantation. Blood 104:865–872
Sorror ML, Sandmaier BM, Storer BE, Maris MB, Baron F, Maloney DG et al (2007) Comorbidity and disease status based risk stratification of outcomes among patients with acute myeloid leukemia or myelodysplasia receiving allogeneic hematopoietic cell transplantation. J Clin Oncol 25:4246–4254
Alessandrino EP, Della Porta MG, Bacigalupo A, Van Lint MT, Falda M, Onida F et al (2008) WHO classification and WPSS predict posttransplantation outcome in patients with myelodysplastic syndrome: a study from the gruppo italiano trapianto di midollo osseo (GITMO). Blood 112:895–902
Warlick ED, Cioc A, Defor T, Dolan M, Weisdorf D (2009) Allogeneic stem cell transplantation for adults with myelodysplastic syndromes: importance of pretransplant disease burden. Biol Blood Marrow Transplant 15:30–38
Lim Z, Brand R, Martino R, van Biezen A, Finke J, Bacigalupo A et al (2010) Allogeneic hematopoietic stem-cell transplantation for patients 50 years or older with myelodysplastic syndromes or secondary acute myeloid leukemia. J Clin Oncol 28:405–411
Lee JH, Lee JH, Lim SN, Kim DY, Kim SH, Lee YS et al (2010) Allogeneic hematopoietic cell transplantation for myelodysplastic syndrome: prognostic significance of pre-transplant IPSS score and comorbidity. Bone Marrow Transplant 45:450–457
Alessandrino EP, Della Porta MG, Bacigalupo A, Malcovati L, Angelucci E, Van Lint MT et al (2010) Prognostic impact of pre-transplantation transfusion history and secondary iron overload in patients with myelodysplastic syndrome undergoing allogeneic stem cell transplantation: a GITMO study. Haematologica 95:476–484
Della Porta MG, Alessandrino EP, Bacigalupo A, van Lint MT, Malcovati L, Pascutto C et al (2014) Predictive factors for the outcome of allogeneic transplantation in patients with MDS stratified according to the revised IPSS-R. Blood 123:2333–2342
Paydas S (2006) Young age MDS: differences between Western and Eastern countries. Leuk Res 30:362
Kuendgen A, Matsuda A, Germing U (2007) Differences in epidemiology of MDS between Western and Eastern countries: ethnic differences or environmental influence? Leuk Res 31:103–104
Sridharan A, Jain R, Bachhuber MA, Yu Y, Ramesh K, Gundabolu K et al (2014) Epidemiologic study of myelodysplastic syndromes in a multiethnic, inner city cohort. Exp Hematol Oncol 3:22
Vardiman JW, Harris NL, Brunning RD (2002) The world health organization (WHO) classification of the myeloid neoplasms. Blood 100:2292–2302
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD et al (2006) Clinical application and proposal for modification of the international working group (IWG) response criteria in myelodysplasia. Blood 108:419–425
Gratwohl A, Hermans J, Niederwieser D, van Biezen A, van Houwelingen HC, Apperley J (2001) Female donors influence transplant-related mortality and relapse incidence in male recipients of sibling blood and marrow transplants. Hematol J 2:363–370
Acknowledgments
The authors thank all the staff involved, including fellow doctors from other specialties, nurses, pharmacists, laboratory, and allied health personnel for their contribution in one way or other to build up the transplant program over the years. Dr. Liyuan Ma is sponsored by the Overseas Training Grant and Young Doctors Talent Development Program of Xinhua Hospital.
Conflict of interest
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Suppl fig 1
OS stratified by aGVHD (present vs absent) (GIF 28 kb)
High resolution image
(TIFF 520 kb)
Suppl fig 2
CIR stratified by IPSS-R (very low/low vs intermediate vs high vs very high risk) (GIF 27 kb)
High resolution image
(TIFF 507 kb)
Suppl fig 3
CIR stratified by cytogenetic groups defined by IPSS-R (very low vs low vs intermediate vs high vs very high risk) (GIF 32 kb)
High resolution image
(TIFF 581 kb)
Suppl fig 4
CIR stratified by cGVHD (present vs absent) (GIF 24 kb)
High resolution image
(TIFF 459 kb)
Suppl fig 5
CINRM stratified by WHO classification (RCUD (RA)/RARS vs RCMD vs RAEB-1 vs RAEB-2) (GIF 27 kb)
High resolution image
(TIFF 455 kb)
Suppl fig 6
CINRM stratified by donor-recipient gender pair (female donor to male recipient vs others) (GIF 27 kb)
High resolution image
(TIFF 435 kb)
Suppl fig 7
CINRM stratified by cGVHD (present vs absent) (GIF 24 kb)
High resolution image
(TIFF 412 kb)
Rights and permissions
About this article
Cite this article
Ma, L., Hao, S., Diong, C. et al. WPSS is a strong prognostic indicator for clinical outcome of allogeneic transplant for myelodysplastic syndrome in Southeast Asian patients. Ann Hematol 94, 761–769 (2015). https://doi.org/10.1007/s00277-014-2275-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-014-2275-x