Abstract
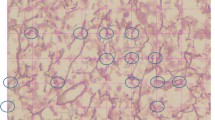
The presence of moderate to severe bone marrow (BM) fibrosis has been shown to be an adverse feature in patients with primary myelodysplastic syndromes (MDS). However, the clinical importance of BM fibrosis is not clear in therapy-related MDS. We retrieved all therapy-related MDS (t-MDS) cases (n = 266) diagnosed at our hospital over a 10-year period (2003–2012). Reticulin and trichrome stains were performed in cases in which BM fibrosis was suspected on initial evaluation of hematoxylin and eosin-stained slide. BM fibrosis was graded according to European consensus guidelines, and a score of MF2/MF3 was defined as moderate/severe fibrosis. Moderate/severe BM fibrosis was found in 47 (17 %) patients. Compared to 219 patients with no/mild BM fibrosis, the patients with moderate/severe fibrosis presented with severer thrombocytopenia (p = 0.039) and higher numbers of circulating blasts (p = 0.051) but with similar degrees of anemia and neutropenia, transfusion requirements, and similar incidences of hepatosplenomegaly and constitutional symptoms. Histological examination revealed a comparable BM cellularity and BM blast percentage, but markedly increased megakaryocytes (p < 0.001) in the fibrotic group. Although the risk distribution of cytogenetic data was similar according to the New Comprehensive Cytogenetic Scoring criteria, −5 and −17 were more frequently observed in t-MDS with moderate/severe BM fibrosis (p = 0.031 and p = 0.043, respectively). With a median follow-up of 11.5 months, patients with moderate/severe BM fibrosis showed a similar risk of acute myeloid leukemia transformation and a comparable overall survival in univariate and multivariate analyses. Moderate/severe BM fibrosis in patients with t-MDS is associated with certain clinicopathological and genetic features. However, unlike the situation in patients with primary MDS, moderate/severe BM fibrosis does not add additional risk to patients with therapy-related MDS.



Similar content being viewed by others
References
Kvasnicka HM, Thiele J, Schmitt-Graeff A, Diehl V, Zankovich R, Niederle N, Leder LD, Schaefer HE (2001) Bone marrow features improve prognostic efficiency in multivariate risk classification of chronic-phase Ph(1+) chronic myelogenous leukemia: a multicenter trial. J Clin Oncol 19(12):2994–3009
Subramanian R, Basu D, Dutta TK (2007) Significance of bone marrow fibrosis in multiple myeloma. Pathology 39(5):512–515. doi:10.1080/00313020701570038
Thiele J, Kvasnicka HM (2005) Hematopathologic findings in chronic idiopathic myelofibrosis. Semin Oncol 32(4):380–394. doi:10.1053/j.seminoncol.2005.04.010
Thiele J, Kvasnicka HM (2006) Grade of bone marrow fibrosis is associated with relevant hematological findings—a clinicopathological study on 865 patients with chronic idiopathic myelofibrosis. Ann Hematol 85(4):226–232. doi:10.1007/s00277-005-0042-8
Vener C, Fracchiolla NS, Gianelli U, Calori R, Radaelli F, Iurlo A, Caberlon S, Gerli G, Boiocchi L, Deliliers GL (2008) Prognostic implications of the European consensus for grading of bone marrow fibrosis in chronic idiopathic myelofibrosis. Blood 111(4):1862–1865. doi:10.1182/blood-2007-09-112953
Gianelli U, Vener C, Bossi A, Cortinovis I, Iurlo A, Fracchiolla NS, Savi F, Moro A, Grifoni F, De Philippis C, Radice T, Bosari S, Lambertenghi Deliliers G, Cortelezzi A (2012) The European Consensus on grading of bone marrow fibrosis allows a better prognostication of patients with primary myelofibrosis. Modern pathology 25(9):1193–1202. doi:10.1038/modpathol.2012.87
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, Harris NL, Le Beau MM, Hellstrom-Lindberg E, Tefferi A, Bloomfield CD (2009) The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114(5):937–951. doi:10.1182/blood-2009-03-209262
Verhoef GE, De Wolf-Peeters C, Ferrant A, Deprez S, Meeus P, Stul M, Zachee P, Cassiman JJ, Van den Berghe H, Boogaerts MA (1991) Myelodysplastic syndromes with bone marrow fibrosis: a myelodysplastic disorder with proliferative features. Ann Hematol 63(5):235–241
Della Porta MG, Malcovati L (2011) Myelodysplastic syndromes with bone marrow fibrosis. Haematologica 96(2):180–183. doi:10.3324/haematol.2010.039875
Buesche G, Teoman H, Wilczak W, Ganser A, Hecker H, Wilkens L, Gohring G, Schlegelberger B, Bock O, Georgii A, Kreipe H (2008) Marrow fibrosis predicts early fatal marrow failure in patients with myelodysplastic syndromes. Leukemia 22(2):313–322. doi:10.1038/sj.leu.2405030
Della Porta MG, Malcovati L, Boveri E, Travaglino E, Pietra D, Pascutto C, Passamonti F, Invernizzi R, Castello A, Magrini U, Lazzarino M, Cazzola M (2009) Clinical relevance of bone marrow fibrosis and CD34-positive cell clusters in primary myelodysplastic syndromes. J Clin Oncol 27(5):754–762. doi:10.1200/JCO.2008.18.2246
Kroger N, Zabelina T, van Biezen A, Brand R, Niederwieser D, Martino R, Lim ZY, Onida F, Schmid C, Garderet L, Robin M, van Gelder M, Marks R, Symeonidis A, Kobbe G, de Witte T (2011) Allogeneic stem cell transplantation for myelodysplastic syndromes with bone marrow fibrosis. Haematologica 96(2):291–297. doi:10.3324/haematol.2010.031229
Voso MT, D’Alo F, Greco M, Fabiani E, Criscuolo M, Migliara G, Pagano L, Fianchi L, Guidi F, Hohaus S, Leone G (2010) Epigenetic changes in therapy-related MDS/AML. Chemico-biological interactions 184(1–2):46–49. doi:10.1016/j.cbi.2009.10.013
Greco M, D’Alo F, Scardocci A, Criscuolo M, Fabiani E, Guidi F, Di Ruscio A, Migliara G, Pagano L, Fianchi L, Chiusolo P, Hohaus S, Leone G, Voso MT (2010) Promoter methylation of DAPK1, E-cadherin and thrombospondin-1 in de novo and therapy-related myeloid neoplasms. Blood cells, molecules & diseases 45(3):181–185. doi:10.1016/j.bcmd.2010.05.008
Li L, Li M, Sun C, Francisco L, Chakraborty S, Sabado M, McDonald T, Gyorffy J, Chang K, Wang S, Fan W, Li J, Zhao LP, Radich J, Forman S, Bhatia S, Bhatia R (2011) Altered hematopoietic cell gene expression precedes development of therapy-related myelodysplasia/acute myeloid leukemia and identifies patients at risk. Cancer cell 20(5):591–605. doi:10.1016/j.ccr.2011.09.011
Christiansen DH, Andersen MK, Desta F, Pedersen-Bjergaard J (2005) Mutations of genes in the receptor tyrosine kinase (RTK)/RAS-BRAF signal transduction pathway in therapy-related myelodysplasia and acute myeloid leukemia. Leukemia 19(12):2232–2240. doi:10.1038/sj.leu.2404009
Singh ZN, Huo D, Anastasi J, Smith SM, Karrison T, Le Beau MM, Larson RA, Vardiman JW (2007) Therapy-related myelodysplastic syndrome: morphologic subclassification may not be clinically relevant. Am J Clin Pathol 127(2):197–205. doi:10.1309/NQ3PMV4U8YV39JWJ
Vardiman JW, Arber DA, Brunning RD, Larson RA, Matutes E, Baumann I, Thiele J (eds) (2008) Therapy-related myeloid neoplasms. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. International Agency for Research on Cancer (IARC), vol 184, 4th edn. Elsevier, Lyon, pp 16–20
Klyuchnikov E, Holler E, Bornhauser M, Kobbe G, Nagler A, Shimoni A, Konecke C, Wolschke C, Bacher U, Zander AR, Kroger N (2012) Donor lymphocyte infusions and second transplantation as salvage treatment for relapsed myelofibrosis after reduced-intensity allografting. Br J Haematol. doi:10.1111/bjh.12013
Quintas-Cardama AKH, Shan J, Jabbour E, Faderl S, Wierda WG, RavandiF KT, Wang SA, Pierce S, Kantarjian HM, Garcia-Manero G (2012) A prognostic model of therapy-related myelodysplastic syndrome for predicting survival and transformation to acute myeloid leukemia. Blood 118(suppl 1):967
Thiele J, Kvasnicka HM, Facchetti F, Franco V, van der Walt J, Orazi A (2005) European consensus on grading bone marrow fibrosis and assessment of cellularity. Haematologica 90(8):1128–1132
Khoury JD, Sen F, Abruzzo LV, Hayes K, Glassman A, Medeiros LJ (2003) Cytogenetic findings in blastoid mantle cell lymphoma. Hum Pathol 34(10):1022–1029
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, Bennett JM, Bowen D, Fenaux P, Dreyfus F, Kantarjian H, Kuendgen A, Levis A, Malcovati L, Cazzola M, Cermak J, Fonatsch C, Le Beau MM, Slovak ML, Krieger O, Luebbert M, Maciejewski J, Magalhaes SM, Miyazaki Y, Pfeilstocker M, Sekeres M, Sperr WR, Stauder R, Tauro S, Valent P, Vallespi T, van de Loosdrecht AA, Germing U, Haase D (2012) Revised international prognostic scoring system for myelodysplastic syndromes. Blood 120(12):2454–2465. doi:10.1182/blood-2012-03-420489
Schanz J, Tuchler H, Sole F, Mallo M, Luno E, Cervera J, Granada I, Hildebrandt B, Slovak ML, Ohyashiki K, Steidl C, Fonatsch C, Pfeilstocker M, Nosslinger T, Valent P, Giagounidis A, Aul C, Lubbert M, Stauder R, Krieger O, Garcia-Manero G, Faderl S, Pierce S, Le Beau MM, Bennett JM, Greenberg P, Germing U, Haase D (2012) New comprehensive cytogenetic scoring system for primary myelodysplastic syndromes (MDS) and oligoblastic acute myeloid leukemia after MDS derived from an international database merge. J Clin Oncol 30(8):820–829. doi:10.1200/JCO.2011.35.6394
Chen W, Konoplev S, Medeiros LJ, Koeppen H, Leventaki V, Vadhan-Raj S, Jones D, Kantarjian HM, Falini B, Bueso-Ramos CE (2009) Cuplike nuclei (prominent nuclear invaginations) in acute myeloid leukemia are highly associated with FLT3 internal tandem duplication and NPM1 mutation. Cancer 115(23):5481–5489. doi:10.1002/cncr.24610
Millecker L, Lennon PA, Verstovsek S, Barkoh B, Galbincea J, Hu P, Chen SS, Jones D (2010) Distinct patterns of cytogenetic and clinical progression in chronic myeloproliferative neoplasms with or without JAK2 or MPL mutations. Cancer genetics and cytogenetics 197(1):1–7. doi:10.1016/j.cancergencyto.2009.10.014
Gustafson SA, Lin P, Chen SS, Chen L, Abruzzo LV, Luthra R, Medeiros LJ, Wang SA (2009) Therapy-related acute myeloid leukemia with t (8;21) (q22;q22) shares many features with de novo acute myeloid leukemia with t (8;21)(q22;q22) but does not have a favorable outcome. Am J Clin Pathol 131(5):647–655. doi:10.1309/AJCP5ETHDXO6NCGZ
Tefferi A (2005) Pathogenesis of myelofibrosis with myeloid metaplasia. J Clin Oncol 23(33):8520–8530. doi:10.1200/JCO.2004.00.9316
Kanagal-Shamanna R, Bueso-Ramos CE, Barkoh B, Lu G, Wang S, Garcia-Manero G, Vadhan-Raj S, Hoehn D, Medeiros LJ, Yin CC (2012) Myeloid neoplasms with isolated isochromosome 17q represent a clinicopathologic entity associated with myelodysplastic/myeloproliferative features, a high risk of leukemic transformation, and wild-type TP53. Cancer 118(11):2879–2888. doi:10.1002/cncr.26537
Hussein K, Van Dyke DL, Tefferi A (2009) Conventional cytogenetics in myelofibrosis: literature review and discussion. Eur J Haematol 82(5):329–338. doi:10.1111/j.1600-0609.2009.01224.x
Mesa RA, Li CY, Ketterling RP, Schroeder GS, Knudson RA, Tefferi A (2005) Leukemic transformation in myelofibrosis with myeloid metaplasia: a single-institution experience with 91 cases. Blood 105(3):973–977. doi:10.1182/blood-2004-07-2864
Barosi G, Bergamaschi G, Marchetti M, Vannucchi AM, Guglielmelli P, Antonioli E, Massa M, Rosti V, Campanelli R, Villani L, Viarengo G, Gattoni E, Gerli G, Specchia G, Tinelli C, Rambaldi A, Barbui T (2007) JAK2 V617F mutational status predicts progression to large splenomegaly and leukemic transformation in primary myelofibrosis. Blood 110(12):4030–4036. doi:10.1182/blood-2007-07-099184
Klimek VM, Dolezal EK, Tees MT, Devlin SM, Stein K, Romero A, Nimer SD (2012) Efficacy of hypomethylating agents in therapy-related myelodysplastic syndromes. Leuk Res 36(9):1093–1097. doi:10.1016/j.leukres.2012.04.025
Breccia M, Salaroli A, Loglisci G, Martelli M, D’Elia GM, Nanni M, Mauro FR, Alimena G (2011) 5′-Azacitidine for therapy-related myelodysplastic syndromes after non-Hodgkin lymphoma treatment. Leuk Res 35(10):1409–1411. doi:10.1016/j.leukres.2011.05.030
Buhr T, Busche G, Choritz H, Langer F, Kreipe H (2003) Evolution of myelofibrosis in chronic idiopathic myelofibrosis as evidenced in sequential bone marrow biopsy specimens. Am J Clin Pathol 119(1):152–158. doi:10.1309/PTVG-B3DX-B8A8-M7KD
Morel F, Le Bris MJ, Herry A, Morice P, De Braekeleer M (2003) Trisomy 15 as the sole abnormality in myelodysplastic syndromes: case report and review of the literature. Leukemia & lymphoma 44(3):549–551. doi:10.1080/1042819021000055084
Conflict of interest
The authors declare that they have no competing interests.
Authors’ information
BF and WX conducted this study as visiting scholars at The University of Texas M.D. Anderson Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Additional information
Informed consent was obtained from all patients for being included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Fu, B., Ok, C.Y., Goswami, M. et al. The clinical importance of moderate/severe bone marrow fibrosis in patients with therapy-related myelodysplastic syndromes. Ann Hematol 92, 1335–1343 (2013). https://doi.org/10.1007/s00277-013-1776-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-013-1776-3