Abstract
Purpose
The open Trillat Procedure described to treat recurrent shoulder instability, has a renewed interest with the advent of arthroscopy. The suprascapular nerve (SSN) is theoretically at risk during the drilling of the scapula near the spinoglenoid notch. The purpose of this study was to assess the relationship between the screw securing the coracoid transfer and the SSN during open Trillat Procedure and define a safe zone for the SSN.
Methods
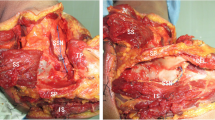
In this anatomical study, an open Trillat Procedure was performed on ten shoulders specimens. The coracoid was fixed by a screw after partial osteotomy and antero-posterior drilling of the scapular neck. The SSN was dissected with identification of the screw. We measured the distances SSN-screw (distance 1) and SSN-glenoid rim (distance 2). In axial plane, we measured the angles between the glenoid plane and the screw (α angle) and between the glenoid plane and the SSN (β angle).
Results
The mean distance SSN-screw was 8.8 mm +/-5.4 (0–15). Mean α angle was 11°+/-2.4 (8–15). Mean β angle was 22°+/-6.7 (12–30). No macroscopic lesion of the SSN was recorded but in 20% (2 cases), the screw was in contact with the nerve. In both cases, the β angle was measured at 12°.
Conclusion
During the open Trillat Procedure, the SSN can be injured due to its anatomical location. Placement of the screw should be within 10° of the glenoid plane to minimize the risk of SSN injury and could require the use of a specific guide or arthroscopic-assisted surgery.







Similar content being viewed by others
Data availability
Not applicable.
Abbreviations
- BMI:
-
Body Mass Index
- SSN:
-
Suprascapular Nerve
- SD:
-
Standard Deviation
References
Albritton MJ, Graham RD, Richards RS, Basamania CJ (2003) An anatomic study of the effects on the suprascapular nerve due to retraction of the supraspinatus muscle after a rotator cuff tear. J Shoulder Elb Surg 12:497–500. https://doi.org/10.1016/S1058-2746(03)00182-4
Bigliani LU, Dalsey RM, McCann PD, April EW (1990) An anatomical study of the suprascapular nerve. Arthroscopy: J Arthroscopic & Related Surg 6:301–305. https://doi.org/10.1016/0749-8063(90)90060-Q
Boileau P, Clowez G, Bouacida S, Walch G, Trojani C, Schwartz DG (2023) The arthroscopic Trillat Procedure is a Valuable Treatment option for recurrent anterior instability in young athletes with shoulder hyperlaxity. Arthroscopy: J Arthroscopic Relat Surg 39:948–958. https://doi.org/10.1016/j.arthro.2022.10.046
Butt U, Charalambous CP (2012) Complications associated with open coracoid transfer procedures for shoulder instability. J Shoulder Elb Surg 21:1110–1119. https://doi.org/10.1016/j.jse.2012.02.008
Chauvet T, Labattut L, Colombi R, Baudin F, Baulot E, Martz P (2022) Arthroscopic trillat technique for chronic post-traumatic anterior shoulder instability: outcomes at 2 years of follow-up. J Shoulder Elb Surg 31:e270–e278. https://doi.org/10.1016/j.jse.2021.12.007
De Mulder K, Marynissen H, Van Laere C, Lagae K, Declercq G (1998) Arthroscopic transglenoid suture of Bankart lesions. Acta Orthop Belg 64:160–166
Duparc F, Coquerel D, Ozeel J, Noyon M, Gerometta A, Michot C (2010) Anatomical basis of the suprascapular nerve entrapment, and clinical relevance of the supraspinatus fascia. Surg Radiol Anat 32:277–284. https://doi.org/10.1007/s00276-010-0631-7
Gerber C, Terrier F, Ganz R (1988) The Trillat procedure for recurrent anterior instability of the shoulder. J Bone Joint Surg Br Volume 70–B:130–134. https://doi.org/10.1302/0301-620X.70B1.3339045
Gumina S, Albino P, Giaracuni M, Vestri A, Ripani M, Postacchini F (2011) The safe zone for avoiding suprascapular nerve injury during shoulder arthroscopy: an anatomical study on 500 dry scapulae. J Shoulder Elb Surg 20:1317–1322. https://doi.org/10.1016/j.jse.2011.01.033
Hernandez A, Drez D (1986) Operative treatment of posterior shoulder dislocations by posterior glenoidplasty, capsulorrhaphy, and infraspinatus advancement. Am J Sports Med 14:187–191. https://doi.org/10.1177/036354658601400301
Housset V, Chevallier R, Nourissat G (2021) Open Trillat Procedure for recurrent anterior instability of the shoulder in Elderly patients. Arthrosc Techniques 10(5):e1211–e1216. https://doi.org/10.1016/j.eats.2021.01.021
Hurley ET, Lim Fat D, Farrington SK, Mullett H (2019) Open Versus Arthroscopic Latarjet Procedure for Anterior Shoulder instability: a systematic review and Meta-analysis. Am J Sports Med 47:1248–1253. https://doi.org/10.1177/0363546518759540
Jouve F, Graveleau N, Nové-Josserand L, Walch G (2008) Recurrent anterior instability of the shoulder associated with full thickness rotator cuff tear: results of surgical treatment. Rev Chir Orthop Reparatrice Appar Mot 94:659–669. https://doi.org/10.1016/j.rco.2008.03.032
Kazum E, Martinez-Catalan N, Oussama R, Eichinger JK, Werthel JD, Valenti P (2022) Arthroscopic trillat procedure combined with capsuloplasty: an effective treatment modality for shoulder instability associated with hyperlaxity. Knee Surg Sports Traumatol Arthrosc 30:2067–2073. https://doi.org/10.1007/s00167-021-06752-z
Labattut L, Chauvet T, Colombi R, Baulot E, Martz P (2021) What did we learn from our first arthroscopic trillat procedures? Results, complications and failures in a series of 100 anterior shoulder stabilizations. Orthop J Sports Med 9(2 Suppl):2325967121S00005. https://doi.org/10.1177/2325967121S00005
Lädermann A, Denard PJ, Burkhart SS (2012) Injury of the Suprascapular Nerve During Latarjet Procedure: An Anatomic Study. Arthroscopy: J Arthroscopic & Related Surg 28:316–321. https://doi.org/10.1016/j.arthro.2011.08.307
Loirat M-A, Tierny M, Hervé A, Lignel A, Berton E, Ropars M, Thomazeau H (2017) A new approach for endoscopic neurolysis of the suprascapular nerve at the spinoglenoid notch: a preliminary cadaver study. Orthop Traumatol: Surg Res 103:861–864. https://doi.org/10.1016/j.otsr.2017.04.011
Longo UG, Forriol F, Loppini M, Lanotte A, Salvatore G, Maffulli N, Denaro V (2015) The safe zone for avoiding suprascapular nerve injury in bone block procedures for shoulder instability. A cadaveric study. Knee Surg Sports Traumatol Arthrosc 23:1506–1510. https://doi.org/10.1007/s00167-014-2900-1
Maquieira GJ, Gerber C, Schneeberger AG (2007) Suprascapular nerve palsy after the Latarjet procedure. J Shoulder Elb Surg 16:e13–e15. https://doi.org/10.1016/j.jse.2006.04.001
Mologne TS, Lapoint JM, Morin WD, Zilberfarb J, O’Brien TJ (1996) Arthroscopic anterior Labral Reconstruction using a Transglenoid suture technique: results in active-duty military patients. Am J Sports Med 24:268–274. https://doi.org/10.1177/036354659602400304
Plancher KD, Petterson SC (2014) Posterior shoulder Pain and arthroscopic decompression of the Suprascapular nerve at the Spinoglenoid Notch. Oper Tech Sports Med 22:73–87. https://doi.org/10.1053/j.otsm.2014.06.001
Reddy Sangam M (2013) A study on the morphology of the Suprascapular Notch and its Distance from the glenoid cavity. J Clin Diagnosis Res 7:189–192. https://doi.org/10.7860/JCDR/2013/4838.2723
Sastre S, Peidro L, Méndez A, Calvo E (2016) Suprascapular nerve palsy after arthroscopic latarjet procedure: a case report and review of literature. Knee Surg Sports Traumatol Arthrosc 24:601–603. https://doi.org/10.1007/s00167-014-3075-5
Shishido H, Kikuchi S (2001) Injury of the suprascapular nerve in shoulder surgery: an anatomic study. J Shoulder Elb Surg 10:372–376. https://doi.org/10.1067/mse.2001.115988
Swan J, Boileau P, Barth J (2020) Arthroscopic Trillat Procedure: a guided technique. Arthrosc Techniques 9:e513–e519. https://doi.org/10.1016/j.eats.2019.12.004
Trillat A (1954) Treatment of recurrent dislocation of the shoulder; technical considerations. Lyon Chir 49:986–993
Valenti P, Maroun C, Schoch B, Arango SO, Werthel J-D (2019) Arthroscopic trillat coracoid transfer Procedure using a cortical button for chronic anterior shoulder instability. Arthrosc Techniques 8:e199–e204. https://doi.org/10.1016/j.eats.2018.10.013
Velasquez Garcia A, Chaney GK, Ingala Martini L, Valenti P (2022) The Trillat Procedure for Anterior Glenohumeral instability. J Bone Joint Surg Reviews 10(8). e22.00049
Walch G, Dejour H, Trillat AG (1987) Recurrent anterior luxation of the shoulder occurring after the age of 40. Rev Chir Orthop Reparatrice Appar Mot 73:609–616
Warner JP, Krushell RJ, Masquelet A, Gerber C (1992) Anatomy and relationships of the suprascapular nerve: anatomical constraints to mobilization of the supraspinatus and infraspinatus muscles in the management of massive rotator-cuff tears. J Bone Joint Surg 74:36–45. https://doi.org/10.2106/00004623-199274010-00006
Funding
This research did not receive any specific grand from funding agencies in the public, commercial, or not-for-profit sectors. Authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Contributions
LL: data collection, data analysis, manuscript writing. JS: manuscript editing. RBO: data collection. ES: manuscript editing. SL: manuscript editing. SG: protocol development, manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee, the 1964 Helsinki declaration and its later amendments, or comparable ethical standards. This study was exempted from IRB review in accordance with the exemption criteria laid down by the institutional review board of our hospital (Hospices Civils de Lyon, Lyon, France). The Ethics committee did not ask for any consent. Cadavers were obtained from the Anatomy department of Lyon 1 University, which is a French institution that handles cadavers for research and education purposes. None of the authors had access to patient data identifications.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ly, L., Swan, J., Özbek, R.B. et al. Risk of suprascapular nerve injury in open Trillat procedure: an anatomical study. Surg Radiol Anat 46, 451–461 (2024). https://doi.org/10.1007/s00276-024-03337-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-024-03337-6