Abstract
Purpose
Occipital Neuralgia (ON) is defined as a unilateral or bilateral pain in the posterior area of the scalp occurring in the distribution area or areas of the greater occipital nerve (GON), lesser occipital nerve (LON), and/or third occipital nerve (TON). In the present study, the purpose was to show the possible importance of the triangular area (TA) in nerve block applied in ON by measuring the TA between GON, TON, and LON.
Methods
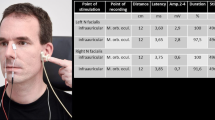
A total of 24 cadavers (14 males, 10 females) were used in the present study. The suboccipital region was dissected, revealing the points where the GON and TON pierced the trapezius muscle and superficial area, and the point where the LON left the sternocleidomastoid muscle from its posterior edge and was photographed. The area of the triangle between the superficial points of these three nerves and the center of gravity of the triangle (CGT) were determined by using the Image J Software and the results were analyzed statistically.
Results
The mean TA values were 952.82 ± 313.36 mm2 and 667.55 ± 273.82 mm2, respectively in male and female cadavers. Although no statistically significant differences were detected between the sides (p > 0.05), a statistically significant difference was detected between the genders (p < 0.05). The mean CGT value was located approximately 5 cm below and 3-3.5 cm laterally from the external occipital protuberance in both genders and sides.
Conclusion
In ON that has more than one occipital nerve involvement, all occipital nerves can be blocked by targeting TA with a single occipital nerve block, and thus, the side effects that may arise from additional blocks can be reduced. The fact that there was a statistically significant difference according to the genders in the TA suggests that different block amounts can be applied according to gender.


Similar content being viewed by others
Consent, data and/or code availability
Not applicable.
References
Anthony M (1992) Headache and the greater occipital nerve. Clin Neurol Neurosurg 94:297–301. https://doi.org/10.1016/0303-8467(92)90177-5
Baek IC, Park K, Kim TL, O J, Yang HM, Kim SH (2018) Comparing the injectate spread and nerve involvement between different injectate volumes for ultrasound-guided greater occipital nerve block at the C2 level: a cadaveric evaluation. J Pain Res 11:2033–2038. https://doi.org/10.2147/JPR.S172692
Barut C, Dogan A, Buyukuysal MC (2014) Anthropometric aspects of hand morphology in relation to sex and to body mass in a Turkish population sample. Homo 65:338–348. https://doi.org/10.1016/j.jchb.2014.03.004
Cesmebasi A, Muhleman MA, Hulsberg P, Gielecki J, Matusz P, Tubbs RS et al (2015) Occipital neuralgia: anatomic considerations. Clin Anat 28:101–108. https://doi.org/10.1002/ca.22468
Classification of chronic pain (1986) Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 3:S1–226
Djavaherian DM, Guthmiller KB (2023) Occipital neuralgia. StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL)
Dougherty C (2014) Occipital neuralgia. Curr Pain Headache Rep 18:411. https://doi.org/10.1007/s11916-014-0411-x
Ducic I, Hartmann EC, Larson EE (2009) Indications and outcomes for surgical treatment of patients with chronic migraine headaches caused by occipital neuralgia. Plast Reconst Surg 123:1453–1461. https://doi.org/10.1097/PRS.0b013e3181a0720e
Geeta A, Jamaiyah H, Safiza MN, Khor GL, Kee CC, Ahmad AZ et al (2009) Reliability, technical error of measurements and validity of instruments for nutritional status assessment of adults in Malaysia. Singap Med J 50:1013–1018
Guyuron B, Kriegler JS, Davis J, Amini SB (2005) Comprehensive surgical treatment of migraine headaches. Plast Reconst Surg 115:1–9. https://doi.org/10.1097/01.PRS.0000145631.20901.84
Headache Classification Committee of the International Headache Society (2018) The International classification of Headache disorders: 3rd edition. Cephalalgia 38(1–211). https://doi.org/10.1177/0333102417738202
Juškys R, Šustickas G (2018) Effectiveness of treatment of occipital neuralgia using the nerve block technique: a prospective analysis of 44 patients. Acta Med Litu 25:53–60. https://doi.org/10.6001/actamedica.v25i2.3757
Kapoor V, Rothfus WE, Grahovac SZ, Amin Kassam SZ, Horowitz MB (2003) Refractory occipital neuralgia: preoperative assessment with CT-guided nerve block prior to dorsal cervical rhizotomy. Am J Neuroradiol 24:2105–2110
Kapural L, Mekhail N, Hayek SM, Stanton-Hicks M, Malak O (2005) Occipital nerve electrical stimulation via the midline approach and subcutaneous surgical leads for treatment of severe occipital neuralgia: a pilot study. Anesth Analg 101:171–174. https://doi.org/10.1213/01.ANE.0000156207.73396.8E
Kemper CJ, Schwerdtfeger A (2009) Comparing indirect methods of digit ratio (2D:4D) measurement. Am J Hum Biol 21:188–191. https://doi.org/10.1002/ajhb.20843
Kuhn WF, Kuhn SC, Gilberstadt H (1997) Occipital neuralgias: clinical recognition of a complicated headache. A case series and literature review. J Orofac Pain 11:158–165
Lainé G, Jecko V, Wavasseur T, Gimbert E, Vignes JR, Liguoro D (2022) Anatomy of the greater occipital nerve: implications in posterior fossa approaches. Surg Radiol Anat 44:573–583. https://doi.org/10.1007/s00276-022-02906-x
Lavin PJ, Workman R (2001) Cushing syndrome induced by serial occipital nerve blocks containing corticosteroids. Headache 41:902–904. https://doi.org/10.1111/j.1526-4610.2001.01165.x
Mathew PG, Najib U, Khaled S, Krel R (2021) Prevalence of Occipital Neuralgia at a Community Hospital-based Headache Clinic. Neurol Clin Pract 11:6–12. https://doi.org/10.1212/CPJ.0000000000000789
Navani A, Mahajan G, Kreis P, Fishman SM (2006) A case of pulsed radiofrequency lesioning for occipital neuralgia. Pain Med 7:453–456. https://doi.org/10.1111/j.1526-4637.2006.00217.x
Oh MY, Ortega J, Bellotte JB, Whiting DM, Aló K (2004) Peripheral nerve stimulation for the treatment of occipital neuralgia and transformed migraine using a C1-2-3 subcutaneous paddle style electrode: a technical report. Neuromodulation 7:103–112. https://doi.org/10.1111/j.1094-7159.2004.04014.x
Poletti CE (1983) Proposed operation for occipital neuralgia: C-2 and C-3 root decompression. Case report. Neurosurgery 12:221–224. https://doi.org/10.1227/00006123-198302000-00017
Sahai-Srivastava S, Subhani D (2010) Adverse effect profile of lidocaine injections for occipital nerve block in occipital neuralgia. J Headache Pain 11:519–523. https://doi.org/10.1007/s10194-010-0244-x
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9:671–675. https://doi.org/10.1038/nmeth.2089
Sharma RR, Devadas RV, Pawar SJ, Lad SD, Mahapatra AK (2005) Current status of peripheral neurectomy for occipital neuralgia. Neurosurg Q 15:232–238. https://doi.org/10.1097/01.wnq.0000190410.48287.30
Song Z, Zhao S, Ma J, Wu Z, Yang S (2020) Fluoroscopy-guided blockade of the Greater Occipital nerve in Cadavers: a comparison of spread and nerve involvement for different Injectate volumes. Pain Res Manag 2020:8925895. https://doi.org/10.1155/2020/8925895
Stechison MT, Mullin BB (1994) Surgical treatment of greater occipital neuralgia: an appraisal of strategies. Acta Neurochir (Wien) 131:236–240. https://doi.org/10.1007/BF01808620
Sunderland E (1995) Anthropometry: the individual and the Population. J Med Genet 32:582
Voigt CL, Murphy MO (2015) Occipital nerve blocks in the treatment of headaches: safety and efficacy. J Emerg Med 48:115–129. https://doi.org/10.1016/j.jemermed.2014.09.007
Wang MY, Levi AD (2002) Ganglionectomy of C-2 for the treatment of medically refractory occipital neuralgia. Neurosurg Focus 12:1–3. https://doi.org/10.3171/foc.2002.12.1.15
Weinberg SM, Scott NM, Neiswanger K, Marazita ML (2005) Intraobserver error associated with measurements of the hand. Am J Hum Biol 17:368–371. https://doi.org/10.1002/ajhb.20129
Acknowledgements
We are eternally grateful to our cadavers for their sacrifice and to their precious families for their patience.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
L.S. and A. K. wrote the main manuscript text. O. C. and Ö. G. collected and analyzed the data, and edited the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Clinical Research Ethical Committee of Istanbul Faculty of Medicine, Istanbul University (Date: 05/03/2021, No: 06).
Consent to participate and/or Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sağlam, L., Gayretli, Ö., Coşkun, O. et al. The triangular area between the greater, lesser, and third occipital nerves and its possible clinical significance. Surg Radiol Anat 46, 185–190 (2024). https://doi.org/10.1007/s00276-024-03307-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-024-03307-y