Abstract
Background
Evaluation of the cystic duct anatomy prior to bile duct or gallbladder surgery is important, to decrease the risk of bile duct injury. This study aimed to clarify the frequency of cystic duct variations and the relationship between them.
Methods
Data of 205 patients who underwent cholecystectomy after imaging at Sada Hospital, Japan, were analyzed. The Chi-square test was used to analyze the relationships among variations.
Results
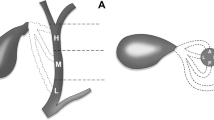
The lateral and posterior sides of the bile duct were the two most common insertion points (92 patients, 44.9%), and the middle height was the most common insertion height (135 patients, 65.9%). Clinically important variations (spiral courses, parallel courses, low insertions, and right hepatic duct draining) relating to the risk of bile duct injury were observed in 24 patients (11.7%). Regarding the relationship between the insertion sides and heights, we noticed that the posterior insertion frequently existed in low insertions (75.0%, P < 0.001) and did not exist in high insertions. In contrast, the anterior insertion coexisted with high and never low insertions. Spiral courses have two courses: anterior and posterior, and anterior ones were only found in high insertion cases.
Conclusions
The insertion point of the cystic duct and the spiral courses tended to be anterior or lateral superiorly and posterior inferiorly. Clinically significant variations in cystic duct insertions are common and surgeons should be cautious about these variations to avoid complications.





Similar content being viewed by others
Data availability
There are ethical restrictions on sharing an original anonymized data set, because the data contain potentially identifying patient information; origin of patients and operation dates. After the approval of the IRB, the data can be provided. Contact the corresponding author, Kenji Fujiwara.
References
Aljiffry M, Abbas M, Wazzan MAM et al (2020) Biliary anatomy and pancreatic duct variations: a cross-sectional study. Saudi J Gastroenterol 26:188–193. https://doi.org/10.4103/sjg.SJG_573_19
Barrett M, Asbun HJ, Chien HL et al (2018) Bile duct injury and morbidity following cholecystectomy: a need for improvement. Surg Endosc 32:1683–1688. https://doi.org/10.1007/s00464-017-5847-8
Bonati E, Gnocchi A, Cremaschi E et al (2019) Treatment of postoperative accessory bile duct injury by fibrin glue and balloon tamponade: a case report. Acta Biomed 90:551–555. https://doi.org/10.23750/abm.v90i4.7752
Casabianca AS, Shah MM, Carpizo D (2018) Accessory bile duct: a rare but important anatomical variant. BMJ Case Rep 2018:bcr2018225133. https://doi.org/10.1136/bcr-2018-225133
Fujimoto N, Tomimaru Y, Yamamoto T et al (2020) Clinical investigation of the cystic duct variation based on the anatomy of the hepatic vasculature. Surg Today 50:396–401. https://doi.org/10.1007/s00595-019-01904-8
Gündüz N, Doğan MB, Alacagöz M et al (2021) Anatomical variations of cystic duct insertion and their relationship with choledocholithiasis: an MRCP study. Egypt J Radiol Nucl Med 52:202. https://doi.org/10.1186/s43055-021-00579-x
Gupta V, Jain G (2019) Safe laparoscopic cholecystectomy: adoption of universal culture of safety in cholecystectomy. World J Gastrointest Surg 11:62–84. https://doi.org/10.4240/wjgs.v11.i2.62
Huang TL, Cheng YF, Chen CL et al (1996) Variants of the bile ducts: clinical application in the potential donor of living-related hepatic transplantation. Transplant Proc 28:1669–1670
Hyodo T, Kumano S, Kushihata F et al (2012) CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree. Br J Radiol 85:887–896. https://doi.org/10.1259/bjr/21209407
Järhult J (2005) Is preoperative evaluation of the biliary tree necessary in uncomplicated gallstone disease? Results of a randomized trial. Scand J Surg 94:31–33. https://doi.org/10.1177/145749690509400108
Kubota Y, Yamaguchi T, Tani K et al (1993) Anatomical variation of pancreatobiliary ducts in biliary stone diseases. Abdom Imaging 18:145–149. https://doi.org/10.1007/BF00198052
Lau WY, Lai ECH, Lau SHY (2010) Management of bile duct injury after laparoscopic cholecystectomy: a review. ANZ J Surg 80:75–81. https://doi.org/10.1111/j.1445-2197.2009.05205.x
Meulepas JM, Ronckers CM, Smets AMJB et al (2019) Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer Inst 111:256–263. https://doi.org/10.1093/jnci/djy104
Miyakawa T (1980) The clinical significance of accessory bile duct: evaluation with PTC and ERCP. Japanese J Gastroenterol Surg 13:451–458. https://doi.org/10.5833/jjgs.13.6_451
Ohana O, Soffer S, Zimlichman E, Klang E (2018) Overuse of CT and MRI in paediatric emergency departments. Br J Radiol 91:20170434. https://doi.org/10.1259/bjr.20170434
Pavlidis TE, Triantafyllou A, Psarras K et al (2008) Long, parallel cystic duct in laparoscopic cholecystectomy for acute cholecystitis: the role of magnetic resonance cholangiopancreatography. JSLS J Soc Laparoendosc Surg 12:407–409
Pesce A, La Greca G, Esposto Ultimo L et al (2020) Effectiveness of near-infrared fluorescent cholangiography in the identification of cystic duct-common hepatic duct anatomy in comparison to magnetic resonance cholangio-pancreatography: a preliminary study. Surg Endosc 34:2715–2721. https://doi.org/10.1007/s00464-019-07158-2
Puente SG, Bannura GC (1983) Radiological anatomy of the biliary tract: variations and congenital abnormalities. World J Surg 7:271–276. https://doi.org/10.1007/BF01656159
Sarawagi R, Sundar S, Gupta SK, Raghuwanshi S (2016) Anatomical variations of cystic ducts in magnetic resonance cholangiopancreatography and clinical implications. Radiol Res Pract 2016:3021484FRPSD. https://doi.org/10.1155/2016/3021484
Sarawagi R, Sundar S, Raghuvanshi S et al (2016) Common and uncommon anatomical variants of intrahepatic bile ducts in magnetic resonance cholangiopancreatography and its clinical implication. Polish J Radiol 81:250–255. https://doi.org/10.12659/PJR.895827
Shimizu Y, Otani T, Matsumoto J et al (2014) Cystic duct with no visible signal on magnetic resonance cholangiography is associated with laparoscopic difficulties: an analysis of 695 cases. Surg Today 44:1490–1495. https://doi.org/10.1007/s00595-013-0715-1
Tringali A, Massinha P, Schepis T et al (2020) Long-term outcomes of endoscopic treatment of aberrant hepatic duct injuries after cholecystectomy. Gastrointest Endosc 91:584–592. https://doi.org/10.1016/j.gie.2019.09.043
Turner MA, Fulcher AS (2001) The cystic duct: normal anatomy and disease processes. Radiographics 21:3–22. https://doi.org/10.1148/radiographics.21.1.g01ja093
Wakabayashi G, Iwashita Y, Hibi T et al (2018) Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 25:73–86
Yabe S, Nakagawa T, Okumura K et al (2020) Preoperative evaluation and management of accessory hepatic ducts for cholecystectomy. Jpn J Gastroenterol Surg 53:399–408. https://doi.org/10.5833/jjgs.2019.0040
Yu MH, Kim YJ, Park HS, Il JS (2020) Benign gallbladder diseases: imaging techniques and tips for differentiating with malignant gallbladder diseases. World J Gastroenterol 26:2967–2986. https://doi.org/10.3748/wjg.v26.i22.2967
Acknowledgements
The authors acknowledge and appreciate the academic support from the Department of Surgery and Oncology, Graduate School of Medical Sciences, Kyushu University. The authors would like to thank Editage (www.editage.com) for English language editing.
Funding
Kenji Fujiwara was supported by KAKENHI under Grant JP20K22817 from the Japan Society for the Promotion of Science. (https://kaken.nii.ac.jp/en/grant/KAKENHI-PROJECT20K22817/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization and data analysis, KF and KH; data curation, KF, AA, TM, TH, and MS; writing, KF, KH, and SK; supervision, MS. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Kenji Fujiwara had consulting fee from Beacon Group Inc., and holds shares at Vanguard. The other authors have declared that no competing interests exist.
Ethical approval
The research was performed in accordance with the Declaration of Helsinki. All data were fully anonymized before the assessment. Our own institutional review board (IRB), Sada Hospital IRB, reviewed and ethically approved the study for the reference of the database and medical records for research purposes. The IRB waived the requirement for informed consent (IRB approval number: S190726-1). Contact form (https://www.sada.or.jp/contact/).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fujiwara, K., Hiraka, K., Shindo, K. et al. Variations in the cystic duct: frequency and the relationship among insertion sides and heights on the bile duct. Surg Radiol Anat 46, 223–230 (2024). https://doi.org/10.1007/s00276-023-03275-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03275-9