Abstract
Purpose
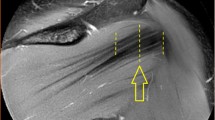
This study aimed to evaluate the morphology of the three parts of the infraspinatus muscle based on surface landmarks for precise and effective access, and to propose the most effective fine-wire electrode insertion technique and sites.
Methods
Fifteen Asian fresh cadavers were used. We investigated the probability of the presence of the superior, middle, and inferior parts in each infraspinatus muscle based on surface landmarks. Based on the positional characteristics of the muscle, we determined the needle insertion method and confirmed its effectiveness by dissection.
Results
The superior part was mostly observed near the spine of the scapula. The middle part was broadly observed within the infraspinous fossa. The inferior part showed variable location within the infraspinous fossa. The injection accuracy of the superior, middle, and inferior parts in the infraspinatus muscle was 95.8%, 100%, and 91.7%, respectively. Targeting the superior and middle parts for injection of the infraspinatus muscle is relatively more straightforward than targeting the inferior part. Targeting the inferior part of the infraspinatus muscle in this study was more challenging than targeting the superior and middle parts.
Conclusion
Needling for electromyography should be performed with special care to avoid unintended muscle parts, which could lead to inaccurate data acquisition and affect the conclusions about muscle function.



Similar content being viewed by others
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request. All data generated or analyzed during this study are included in this published article.
References
Alenabi T, Whittaker R, Kim SY, Dickerson CR (2018) Maximal voluntary isometric contraction tests for normalizing electromyographic data from different regions of supraspinatus and infraspinatus muscles: identifying reliable combinations. J Electromyogr Kinesiol 41:19–26. https://doi.org/10.1016/j.jelekin.2018.04.007
Alenabi T, Whittaker RL, Kim SY, Dickerson CR (2019) Arm posture influences on regional supraspinatus and infraspinatus activation in isometric arm elevation efforts. J Electromyogr Kinesiol 44:108–116. https://doi.org/10.1016/j.jelekin.2018.12.005
Bacle G, Gregoire JM, Patat F, Clavert P, de Pinieux G, Laulan J, Lakhal W, Favard L (2017) Anatomy and relations of the infraspinatus and the teres minor muscles: a fresh cadaver dissection study. Surg Radiol Anat 39:119–126. https://doi.org/10.1007/s00276-016-1707-9
Balbinot G, Joner Wiest M, Li G, Pakosh M, Cesar Furlan J, Kalsi-Ryan S, Zariffa J (2022) The use of surface EMG in neurorehabilitation following traumatic spinal cord injury: a scoping review. Clin Neurophysiol 138:61–73. https://doi.org/10.1016/j.clinph.2022.02.028
Calver R, Alenabi T, Cudlip A, Dickerson CR, Mondal P, Kim SY (2022) Regional activation of supraspinatus and infraspinatus sub-regions during dynamic tasks performed with free weights. J Electromyogr Kinesiol 62:102308. https://doi.org/10.1016/j.jelekin.2019.05.009
Green RA, Pizzari T, McClelland J, Zacharias A, Huynh P, Weerakkody N, Semciw AI (2019) Between session reliability of intramuscular electromyography for segments of gluteus medius and minimus during gait and stepping tasks. J Electromyogr Kinesiol 47:96–104. https://doi.org/10.1016/j.jelekin.2019.05.015
Jandial R, Garfin SR, Ames CP (2012) Best evidence for spine surgery: 20 cardinal cases. Elsevier/Saunders, Philadelphia
Kato A, Nimura A, Yamaguchi K, Mochizuki T, Sugaya H, Akita K (2012) An anatomical study of the transverse part of the infraspinatus muscle that is closely related with the supraspinatus muscle. Surg Radiol Anat 34:257–265. https://doi.org/10.1007/s00276-011-0872-0
Kim SY, Shakeri S, Dickerson CR, Alenabi T, Agur AMR (2019) Verification of intramuscular electromyography electrode placement for neuromuscular partitions of infraspinatus. J Electromyogr Kinesiol 49:102354. https://doi.org/10.1016/j.jelekin.2019.102354
Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW, Group MS (2013) Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg 22:1371–1379. https://doi.org/10.1016/j.jse.2013.01.026
Praagman M, Chadwick EK, van der Helm FC, Veeger HE (2010) The effect of elbow angle and external moment on load sharing of elbow muscles. J Electromyogr Kinesiol 20:912–922. https://doi.org/10.1016/j.jelekin.2010.04.003
Rathi S, Zacharias A, Green RA (2015) Verification of a standardized method for inserting intramuscular electromyography electrodes into teres minor using ultrasound. Clin Anat 28:780–785. https://doi.org/10.1002/ca.22561
Ryan G, Johnston H, Moreside J (2018) Infraspinatus isolation during external rotation exercise at varying degrees of abduction. J Sport Rehabil 27:334–339. https://doi.org/10.1123/jsr.2016-0217
Sasaki S, Kenmoku T, Otera A, Miyajima G, Nagura N, Nakawaki M, Nakazawa T, Takaso M, Fukuda M, Takahira N (2019) Electromyographic analysis of infraspinatus and scapular muscles during external shoulder rotation with different weight loads and positions. J Orthop Sci 24:75–80. https://doi.org/10.1016/j.jos.2018.04.010
Sekiya JK, Safran MR, Ranawat AS, Leunig M (2011) Techniques in hip arthroscopy and joint preservation surgery, 1st edn. Saunders/Elsevier, Philadelphia
Whittaker RL, Alenabi T, Kim SY, Dickerson CR (2022) Regional electromyography of the infraspinatus and supraspinatus muscles during standing isometric external rotation exercises. Sports Health 14:725–732. https://doi.org/10.1177/19417381211043849
Wilk KE, Andrews JR, Arrigo CA (1997) The physical examination of the glenohumeral joint: emphasis on the stabilizing structures. J Orthop Sports Phys Ther 25:380–389. https://doi.org/10.2519/jospt.1997.25.6.380
Wuelker N, Korell M, Thren K (1998) Dynamic glenohumeral joint stability. J Shoulder Elbow Surg 7:43–52. https://doi.org/10.1016/s1058-2746(98)90182-3
Zijdewind I, Thomas CK (2001) Spontaneous motor unit behavior in human thenar muscles after spinal cord injury. Muscle Nerve 24:952–962. https://doi.org/10.1002/mus.1094
Acknowledgements
This study complied with the principles outlined in the Declaration of Helsinki. Consent was received from the families of the deceased patients before beginning the dissections. The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind’s overall knowledge which can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.
Funding
N/A.
Author information
Authors and Affiliations
Contributions
All authors contributed to this study’s conception and design. All authors read and approved the final manuscript. JH-L and KW-L (these authors contributed equally to this work): conceptualization, dissection, experiment, validation, and writing and editing of the original manuscript. KH-Y and HW-H: experiment, validation, and visualization. YJ-C: dissection, experiment, validation, and critical revision of the manuscript for intellectual content. HJ-L: project administration, conceptualization, and supervision. Hyung-Jin Lee is responsible for the overall content as guarantor. All the authors have read and agreed to the publication of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
I acknowledge that I have considered the conflict of interest statement included in the “Author Guidelines.” I hereby certify that, to the best of my knowledge, no aspect of my current personal or professional situation might reasonably be expected to affect my views on the subject I am presenting significantly.
Ethical approval
The study protocol was approved by the Institutional Review Board of the College of Medicine, The Catholic University of Korea (Approval No. MC22SISI0056) and was conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, JH., Lee, KW., Yi, KH. et al. A standardized protocol for needle placement in the infraspinatus muscle: an anatomical perspective. Surg Radiol Anat 45, 1579–1586 (2023). https://doi.org/10.1007/s00276-023-03245-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03245-1