Abstract
Purpose
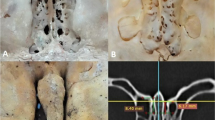
The infratemporal fossa contains important neurovascular components and is directly related to other anatomical regions and structures. The morphometric distances between the bones forming its borders have not been thoroughly investigated. The aim of this study was to determine the morphometry of the infratemporal fossa.
Methods
3D models of the skull of 83 individuals were reconstructed from DICOM datasets, from which length, depth and width measurements were determined and compared between genders and the right and left sides.
Results
All measurements obtained were significantly different between males and females. There were also significant differences between the left and right sides for depth and width measurements.
Conclusion
This is the first study to determine and investigate measurements of the infratemporal fossa; as such it provides a comprehensive view of the morphology of the fossa. It provides valuable information for surgical interventions and differential diagnoses of pathologies in this region, as well as enhancing its understanding in medical education.



Similar content being viewed by others
Data availability
Data sharing not applicable.
References
Adams GL, Gansky SA, Miller AJ, Harrell WE Jr, Hatcher DC (2004) Comparison between traditional 2-dimensional cephalometry and a 3-dimensional approach on human dry skulls. Am J Orthod Dentofacial Orthop 126(4):397–409. https://doi.org/10.1016/j.ajodo.2004.03.023
Boom HP, van Spronsen PH, van Ginkel FC, van Schijndel RA, Castelijns JA, Tuinzing DB (2008) A comparison of human jaw muscle cross-sectional area and volume in long- and short-face subjects, using MRI. Arch Oral Biol 53(3):273–281. https://doi.org/10.1016/j.archoralbio.2007.08.013
Casale J, Bordoni B, Anatomy, head and neck, infratemporal fossa, in Statpearls. 2022: Treasure Island (FL). https://www.ncbi.nlm.nih.gov/books/NBK537034/. Accessed 20 Feb 2023.
De La Pena A, De La Pena-Brambila J, Perez-De La Torre J, Ochoa M, Gallardo GJ (2018) Lowcost customized cranioplasty using a 3D digital printing model a case report. D Print Med. 4(1):4. https://doi.org/10.1186/s41205-018-0026-7
Dumas BM, Nava A, Law HZ, Smartt J, Derderian C, Seaward JR, Kane AA, Hallac RR (2019) Three-dimensional printing for craniofacial surgery: a single institution’s 5-year experience. Cleft Palate Craniofac J 56(6):729–734. https://doi.org/10.1177/1055665618798292
Dwivedi G, Gupta V, Tiwari V, Patnaik U, Sood A, Kumari A, Bharadwaja S (2022) Different approaches to the overlapping infratemporal fossa and parapharyngeal spaces: a case series and review of literature. Indian J Otolaryngol Head Neck Surg 74(Suppl 2):2337–2343. https://doi.org/10.1007/s12070-020-02168-2
Gao L, Zhou L, Dai Z, Huang X (2017) The endoscopic prelacrimal recess approach to the pterygopalatine fossa and infratemporal fossa. J Craniofac Surg 28(6):1589–1593. https://doi.org/10.1097/SCS.0000000000003419
Hosseini SM, Razfar A, Carrau RL, Prevedello DM, Fernandez-Miranda J, Zanation A, Kassam AB (2012) Endonasal transpterygoid approach to the infratemporal fossa: correlation of endoscopic and multiplanar CT anatomy. Head Neck 34(3):313–320. https://doi.org/10.1002/hed.21725
Isolan GR, Rowe R, Al-Mefty O (2007) Microanatomy and surgical approaches to the infratemporal fossa: an anaglyphic three-dimensional stereoscopic printing study. Skull Base 17(5):285–302. https://doi.org/10.1055/s-2007-985193
Joo W, Funaki T, Yoshioka F, Rhoton AL Jr (2013) Microsurgical anatomy of the infratemporal fossa. Clin Anat 26(4):455–469. https://doi.org/10.1002/ca.22202
Kelly RR, Sidles SJ, LaRue AC (2020) Effects of neurological disorders on bone health. Front Psychol 11:6123. https://doi.org/10.3389/fpsyg.2020.612366
Kim TH, Kim CH (2020) Correlation between mandibular morphology and masticatory muscle thickness in normal occlusion and mandibular prognathism. J Korean Assoc Oral Maxillofac Surg 46(5):313–320. https://doi.org/10.5125/jkaoms.2020.46.5.313
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Li L, London NR Jr, Prevedello DM, Carrau RL (2022) Endoscopic endonasal approach to the pterygopalatine fossa and infratemporal fossa: comparison of the prelacrimal and denker’s corridors. Am J Rhinol Allergy 36(5):599–606. https://doi.org/10.1177/19458924221097159
Lim HK, Choi YJ, Choi WC, Song IS, Lee UL (2022) Reconstruction of maxillofacial bone defects using patient-specific long-lasting titanium implants. Sci Rep 12(1):7538. https://doi.org/10.1038/s41598-022-11200-0
Martin CM, Roach VA, Nguyen N, Rice CL, Wilson TD (2013) Comparison of 3D reconstructive technologies used for morphometric research and the translation of knowledge using a decision matrix. Anat Sci Educ 6(6):393–403. https://doi.org/10.1002/ase.1367
Motoike HK, O’Kane RL, Lenchner E, Haspel C (2009) Clay modeling as a method to learn human muscles: a community college study. Anat Sci Educ 2(1):19–23. https://doi.org/10.1002/ase.61
Murgitroyd E, Madurska M, Gonzalez J, Watson A (2015) 3D digital anatomy modelling - practical or pretty? Surgeon 13(3):177–180. https://doi.org/10.1016/j.surge.2014.10.007
Pepicelli A, Woods M, Briggs C (2005) The mandibular muscles and their importance in orthodontics: a contemporary review. Am J Orthod Dentofacial Orthop 128(6):774–780. https://doi.org/10.1016/j.ajodo.2004.09.023
Prades JM, Timoshenko A, Merzougui N, Martin C (2003) A cadaveric study of a combined trans-mandibular and trans-zygomatic approach to the infratemporal fossa. Surg Radiol Anat 25(3–4):180–187. https://doi.org/10.1007/s00276-003-0126-x
Roche PH, Fournier HD, Laccourreye L, Mercier P (2001) Surgical anatomy of the infratemporal fossa using the transmaxillary approach. Surg Radiol Anat 23(4):209–213. https://doi.org/10.1007/s00276-001-0209-5
Rusu MC, Pop F, Curca GC, Podoleanu L, Voinea LM (2009) The pterygopalatine ganglion in humans: a morphological study. Ann Anat 191(2):196–202. https://doi.org/10.1016/j.aanat.2008.09.008
Tessier P, Kawamoto H, Matthews D, Posnick J, Raulo Y, Tulasne JF, Wolfe SA (2005) Autogenous bone grafts and bone substitutes–tools and techniques: I. A 20000-case experience in maxillofacial and craniofacial surgery. Plast Reconstr Surg. 116(5 Suppl):6S-24S. https://doi.org/10.1097/01.prs.0000173862.20563.12
Tiwari R, Quak J, Egeler S, Smeele L, Waal IV, Valk PV, Leemans R (2000) Tumors of the infratemporal fossa. Skull Base Surg 10(1):1–9. https://doi.org/10.1055/s-2000-6789
Toro-Ibacache V, Zapata Munoz V, O’Higgins P (2016) The relationship between skull morphology, masticatory muscle force and cranial skeletal deformation during biting. Ann Anat 203:59–68. https://doi.org/10.1016/j.aanat.2015.03.002
van Vlijmen OJ, Maal T, Berge SJ, Bronkhorst EM, Katsaros C, Kuijpers-Jagtman AM (2010) A comparison between 2D and 3D cephalometry on cbct scans of human skulls. Int J Oral Maxillofac Surg 39(2):156–160. https://doi.org/10.1016/j.ijom.2009.11.017
Vrionis FD, Cano WG, Heilman CB (1996) Microsurgical anatomy of the infratemporal fossa as viewed laterally and superiorly. Neurosurgery 39(4):777–786. https://doi.org/10.1097/00006123-199610000-00027
Weijs WA, Hillen B (1984) Relationships between masticatory muscle cross-section and skull shape. J Dent Res 63(9):1154–1157. https://doi.org/10.1177/00220345840630091201
Witzel U, Preuschoft H (2002) Function-dependent shape characteristics of the human skull. Anthropol Anz 60(2):113–135. https://doi.org/10.1127/anthranz/60/2002/113
You Y, Niu Y, Sun F, Huang S, Ding P, Wang X, Zhang X, Zhang J (2022) Three-dimensional printing and 3D Slicer powerful tools in understanding and treating neurosurgical diseases. Front Surg 9:1030081. https://doi.org/10.3389/fsurg.2022.1030081
Acknowledgements
The authors sincerely thank to technical staff of the Cukurova University Department of Radiology for their technical support and contribution to the collection of CT dataset.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: [HE], [NB], [OO]; Methodology: [HE], [OO]; Formal analysis and investigation: [HE], [NKS]; Writing—original draft preparation: [HE]; Writing—review and editing: [HE], [YC], [RWS]; Resources: [UAP]; Supervision: [OO], [NB]; Visualization: [YC], [HE].
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest. The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Ethical approval was waived by the local Ethics Committee of Cukurova University in view of the retrospective nature of the study and all the procedures being performed were part of the routine care (Protocol no: 6.12.2019/94–18).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Erdem, H., Cevik, Y., Safak, N.K. et al. Morphometric analysis of the infratemporal fossa using three-dimensional (3D) digital models. Surg Radiol Anat 45, 729–734 (2023). https://doi.org/10.1007/s00276-023-03144-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03144-5