Abstract
Purpose
To report atypical anatomical variation of an osseous suprascapular canal, and to elaborate on its clinical significance as a potential anatomical factor that could obscure a direct posterior surgical approach and suprascapular nerve block.
Methods
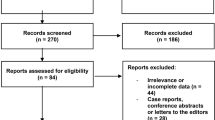
Osteological observational study of the scapula with emphasis on the suprascapular space. The pool of investigated sample size was collectively 768 specimens composed of 529 adult dry scapulae (240 paired, 289 un-paired), 54 children dry scapulae, 135 wet scapulae observed during cadaveric dissections, 47 retrospective 3D CT reconstructions, and 3 retrospective full sequence shoulder MRI. The two reported cases came from the 240 (120 skeleton) observed paired scapulae. Furthermore, the osseous suprascapular canal was examined by X-rays and its internal path was exposed by CT sections. A narrative review was conducted to investigate any relevant reports on the subject matter.
Results
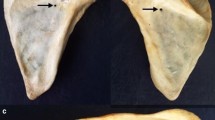
Two left dry bone scapulae with unilateral osseous suprascapular canal were found. The incidence of this atypical morphology of an osseous canal is probably five cases reported in three studies including this cases study.
Conclusions
The reported cases aid in explaining additional possible anatomical factors that could lead to below threshold anesthetic effect in posterior suprascapular nerve block procedures. Therefore, it is more practical to visualize the suprascapular canal by some imaging method before attempting to blindly access the suprascapular nerve in nerve block or posterior surgical approach due to the rare potential existence of an ossified barrier hindering the procedure.
Level of evidence
V Basic Science Research.


Similar content being viewed by others
Availability of data and materials
Not applicable.
References
Al-Redouan A, Holding K, Kachlik D (2021) “Suprascapular canal”: anatomical and topographical description and its clinical implication in entrapment syndrome. Ann Anat 233:151593. https://doi.org/10.1016/j.aanat.2020.151593
Chan CW, Peng PW (2011) Suprascapular nerve block: a narrative review. Reg Anesth Pain Med 36(4):358–373. https://doi.org/10.1097/AAP.0b013e3182204ec0
Cvrček J, Kuželka V, Jor T, Dupej J, Horák M, Naňka O, Brůžek J, Velemínský P (2021) Familial occurrence of skeletal developmental anomalies as a reflection of biological relationships in a genealogically documented Central European sample (19th to 20th centuries). J Anat 239(5):1226–1238. https://doi.org/10.1111/joa.13499
Kamal K, Dahiya N, Singh R, Saini S, Taxak S, Kapoor S (2018) Comparative study of anatomical landmark-guided versus ultrasound-guided suprascapular nerve block in chronic shoulder pain. Saudi J Anaesth 12(1):22–27. https://doi.org/10.4103/sja.SJA_123_17
Kharay SS, Sharma A, Singh P (2016) Unusual morphology of scapulae: incidence and dimensions of ossified ligaments and supraspinous bony tunnels for clinical consideration. Singapore Med J 57(1):29–32
Laumonerie P, Blasco L, Tibbo ME, Panagiotis K, Fernandes O, Lauwers F, Bonnevialle N, Mansat P, Ohl X (2019) Ultrasound-guided versus landmark-based approach to the distal suprascapular nerve block: a comparative cadaveric study. Arthroscopy 35(8):2274–2281. https://doi.org/10.1016/j.arthro.2019.02.050
Leider JD, Derise OC, Bourdreaux KA, Dierks GJ, Lee C, Varrassi G, Sherman WF, Kaye AD (2021) Treatment of suprascapular nerve entrapment syndrome. Orthop Rev (Pavia). 13(2):25554
Pachner P (1937) [Sex differences in the human pelvis]. In Czech. Praha: Czech Academy of Sciences and Arts.
Peng PW, Wiley MJ, Liang J, Bellingham GA (2010) Ultrasound-guided suprascapular nerve block: a correlation with fluoroscopic and cadaveric findings. Can J Anaesth 57(2):143–148. https://doi.org/10.1007/s12630-009-9234-3
Polguj M, Podgórski M, Jędrzejewski K, Topol M (2012) The double suprascapular foramen: unique anatomical variation and the new hypothesis of its formation. Skeletal Radiol 41(12):1631–1636. https://doi.org/10.1007/s00256-012-1460-z
Polguj M, Jędrzejewski K, Topol M (2013) Variable morphology of the anterior coracoscapular ligament—a proposal of classification. Ann Anat 195:77–81. https://doi.org/10.1016/j.aanat.2012.06.003
Schneider-Kolsky ME, Pike J, Connell DA (2004) CT-guided suprascapular nerve blocks: a pilot study. Skeletal Radiol 33(5):277–282. https://doi.org/10.1007/s00256-003-0733-y
Voisin JL, Ropars M, Thomazeau H (2016) Anatomical evidence for a uniquely positioned suprascapular foramen. Surg Radiol Anat 38(4):489–492. https://doi.org/10.1007/s00276-015-1558-9
Yildizgören MT (2020) Ultrasonographic diagnosis and treatment of suprascapular neuropathy secondary to ganglion cyst. J Med Ultrasound 29(3):221–222. https://doi.org/10.4103/JMU.JMU_63_20
Acknowledgements
The authors would like to acknowledge and thank Marek Jantač (Department of Anthropology, National Museum, Prague) for performing the radiographs; Martin Horák (Department of Radiology, Hospital Na Homolce, Prague) for creating the CT scans; Carl V. L. Olson (Department of Anatomy, Second Faculty of Medicine, Charles University, Prague) for his help in taking the specimens photos; Radovan Hudák (Department of Anatomy and Department of Orthopedics, Second Faculty of Medicine, Charles University, Prague) for his help with access to retrospective images; Aimilia Theodorakioglou, Sayed Mehdi Sadat and Michal Benes (Department of Anatomy, Second Faculty of Medicine, Charles University, Prague) for their help with the specimens observations. The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase mankind's overall knowledge that can then improve patient care. Therefore, these donors and their families deserve our highest gratitude.
Funding
This work was supported by The Grant Agency of Charles University (GAUK No. 1720119), and the Ministry of Culture of the Czech Republic (DKRVO 2019–2023/7.I.d, 00023272).
Author information
Authors and Affiliations
Contributions
AA-R: principle researcher, conceptualization, methodology, investigation, visualization, project administration, funding acquisition, writing—original draft. SS: formal analysis. JC: resources, funding acquisition. JV: resources. PV: resources, supervision, visualization. DK: supervision, validation, writing—review and editing. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The ethical and legal access to specimens was approved for research and education purposes by the Institutional Review Board (IRB) The Ethics Committee of the University Hospital Motol and Second Faculty of Medicine, Charles University, in Prague, Czech Republic [Reference ID no. EK-353/19].
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al-Redouan, A., Salavova, S., Cvrček, J. et al. Osseous suprascapular canal: rare variant that would hinder suprascapular nerve block and posterior surgical approach. Surg Radiol Anat 44, 1507–1511 (2022). https://doi.org/10.1007/s00276-022-03045-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-022-03045-z