Abstract
Purpose
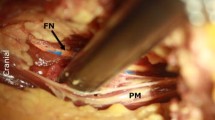
The minimally invasive transpsoas approach can be employed to treat various spinal disorders, such as disc degeneration, deformity, and lateral disc herniation. With this technique, visualization is limited in comparison with the open procedure and the proximity of the lumbar plexus to the surgical pathway is one limitation of this technique. Precise knowledge of the regional anatomy of the lumbar plexus is required for safe passage through the psoas muscle. The primary objective of this study was to determine the anatomic position of the lumbar plexus branches and sympathetic chain in relation to the intervertebral disc and to define a safe working zone. The second objective was to compare our observations with previous anatomical studies concerning the transpsoas approach.
Methods
A total of 60 lumbar plexus in 8 fresh cadavers from the Department of Anatomy were analyzed in this study. Coronal and lateral X-Ray images were obtained before dissection in order to eliminate spine deformity or fracture. All cadavers were placed in a lateral decubitus position with a lateral bolster. Dissection of the lumbar plexus was performed. All nerve branches and sympathetic chain were identified. Intervertebral disc space from L1L2 to L4L5 was divided into four zones. Zone 1 being the anterior quarter of the disc, zone 2 being the middle anterior quarter, zone 3 the posterior middle quarter and zone 4 the posterior quarter. Crossing of each nervous branch with the disc was reported and a safe working zone was determined for L1L2 to L4L5 disc levels. A safe working zone was defined by the absence of crossing of a lumbar plexus branch.
Results
No anatomical variation was found during blunt dissection. As described previously, the lumbar plexus is composed of the ventral divisions of the first four lumbar nerves and from contributions of the sub costal nerve from T12. The safe working zone includes zones 2 and 3 at level L1L2, zone 3 at level L2L3, zone 3 at level L3L4, and zone 2 at level L4L5. No difference was observed between right and left sides as regards the relationships between the lumbar plexus and the intervertebral disc.
Conclusion
We observed some differences concerning the safe working zone in comparison with other cadaveric studies. The small number of cadaveric specimens used in anatomical studies probably explains theses differences. The minimally invasive transpsoas lateral approach was initially developed to reduce the complications associated with the traditional procedure. The anatomical relationships between the lumbar plexus and the intervertebral disc make this technique particularly risky a L4L5. Alternative techniques, such as transforaminal interbody fusion (TLIF), posterior lumbar interbody fusion (PLIF) or anterior interbody fusion (ALIF) should be used at this level.









Similar content being viewed by others
References
Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB (2008) Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech 21:459–467
Banagan K, Gelb D, Poelstra K, Ludwig S (2011) Anatomic mapping of lumbar nerve roots during a direct lateral transpsoas approach to the spine: a cadaveric study. Spine. doi:10.1097/BRS.0b013e3181ec5911
Benglis DM, Vanni S, Levi AD (2009) An anatomical study of the lumbosacral plexus as related to the minimally invasive transpsoas approach to the lumbar spine. J Neurosurg Spine 10:139–144
Bergey DL, Villavicencio AT, Goldstein T, Regan JJ (2004) Endoscopic lateral transpsoas approach to the lumbar spine. Spine 29:1681–1688
Dakwar E, Cardona RF, Smith DA, Uribe JS (2010) Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus 28:E8
Dakwar E, Vale FL, Uribe JS (2011) Trajectory of the main sensory and motor branches of the lumbar plexus outside the psoas muscle related to the latéral retroperitoneal transpsoas approach. J Neurosurg Spine 14:290–295
Fantini GA, Pappou IP, Girardi FP, Sandhu HS, Cammisa FP Jr (2007) Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine 32:2751–2758
Gu Y, Ebraheim NA, Xu R, Rezcallah AT, Yeasting RA (2001) Anatomic considerations of the posterolateral lumbar disk region. Orthopedics 24:56–58
Guérin P, Obeid I, Gille O, Bourghli A, Luc S, Pointillart V, Cursolle JC, Vital JM (2011) Safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: a morphometric study. Surg Radiol Anat. doi:10.1007/s00276-011-0798-6
Hasegawa T, Mikawa Y, Watanabe R, An HS (1996) Morphometric analysis of the lumbosacral nerve roots and dorsal root ganglia by magnetic resonance imaging. Spine 21:1005–1009
Kepler CK, Bogner EA, Herzog RJ, Huang RC (2010) Anatomy of the psoas muscle and lumbar plexus with respect to the surgical approach for lateral transpsoas interbody fusion. Eur Spine J. doi:10.1007/s00586-010-1593-5
Knight RQ, Schwaegler P, Hanscom D, Roh J (2009) Direct lateral lumbar interbody fusion for degenerative conditions: early complication profile. J Spinal Disord Tech 22:34–37
Matejcik V (2010) Anatomical variations of lumbosacral plexus. Surg Radiol Anat 32(4):409–414
Moro T, Kikuchi S, Konno S, Yaginuma H (2003) An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine 28:423–428
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6:435–443
Park DK, Lee MJ, Lin EL, Singh K, An HS, Phillips FM (2010) The relationship of intrapsoas nerves during a transpsoas approach to the lumbar spine: anatomic study. J Spinal Disord Tech 23:223–228
Regev GJ, Chen L, Dhawan M, Lee YP, Garfin SR, Kim CW (2009) Morphometric analysis of the ventral nerve roots and retroperitoneal vessels with respect to the minimally invasive lateral approach in normal and deformed spines. Spine 34:1330–1335
Uribe JS, Arredondo N, Dakwar E, Vale FL (2010) Defining the safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: an anatomical study. J Neurosurg Spine 13:260–266
Acknowledgments
Etienne Delamarre and technicians from Department of Anatomy.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guérin, P., Obeid, I., Bourghli, A. et al. The lumbosacral plexus: anatomic considerations for minimally invasive retroperitoneal transpsoas approach. Surg Radiol Anat 34, 151–157 (2012). https://doi.org/10.1007/s00276-011-0881-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-011-0881-z