Abstract
Purpose
Microspheres are effective embolic agents, especially for the management of bleeding and oncologic lesions. The first FairEmbo study reported the effectiveness of embolization using suture fragments. The effectiveness and safety of arterial embolization with suture-based microparticles (SBM) were assessed in a swine model.
Materials and Methods
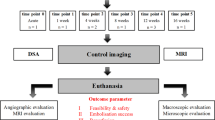
In this ethical-approved animal study, a polar artery in each kidney was embolized in four swine: one side with hand-cut non-absorbable SBM (Flexocrin 2®) and the contralateral side with Embozene® 900 for comparison. Swine were followed for 3 months (M3) to evaluate the effectiveness and the safety of SBM. Follow-up protocol included clinical monitoring, computed tomography (CT) control and digital subtraction angiography (DSA), followed by histological analyses. The SBM confection parameters were evaluated by automatic microscopic sizer. RStudio software and Mann–Whitney test (significance at P < 0.05) were used for statistics.
Results
The average size of SBM was 1002 μm (SD = 258). All targets were effectively embolized by SBM with an angiogram defect estimated at 45.6% (95% CI [35.9–55.2]), compared to 40.5% (95% CI [30.6–55.5]) for Embozene® group (P = 0.342). The average duration of SBM embolization procedure was significantly increased compared to Embozene® embolization (1202 s versus 222 s, P = 0.029). There were no statistical differences in M3 DSA and CT for SBM and Embozene®, with persistence of partial arterial occlusion and atrophic embolized area. No postoperative complications were observed on clinical and CT controls.
Conclusion
This experimental study suggests that embolization with SBM is feasible, safe and effective in short- and medium-term follow-up as compared to microspheres.




Similar content being viewed by others
References
Sharma S, Ganga K. Establishing IR in emerging countries—a skill development initiative. J Vasc Interven Radiol. 2019;30(6):956–60. https://doi.org/10.1016/j.jvir.2018.12.728.
Makris GC, Byrne G. Post-partum hemorrhage and maternal mortality in low-income countries and the forgotten role of interventional radiology. Cardiovasc Interven Radiol. 2019;42(12):1810–1. https://doi.org/10.1007/s00270-019-02339-x.
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33. https://doi.org/10.1016/S2214-109X(14)70227-X.
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386(9995):743–800. https://doi.org/10.1016/S0140-6736(15)60692-4.
Glass Lewis M, Ekúndayò O. Cost and distribution of hysterectomy and uterine artery embolization in the united states: regional/rural/urban disparities. Med Sci. 2017;5(2):10. https://doi.org/10.3390/medsci5020010.
Tang S, A systematic review and meta-analysis of the safety and efficacy of uterine artery embolization vs. surgery for symptomatic uterine fibroids. J Interven Med. 2018; 1(2):9. https://doi.org/https://doi.org/10.19779/j.cnki.2096-3602.2018.02.10.
Vidal V, Hak JF, Brige P, Chopinet S, Tradi F, Bobot M, et al. In Vivo feasibility of arterial embolization with permanent and absorbable suture: the fair-embo concept. Cardiovasc Intervent Radiol. 2019;42(8):1175–82. https://doi.org/10.1007/s00270-019-02211-y.
Diop AD, Diop AN, Hak JF, Di Bisceglie M, Bartoli JM, Guillet B, Vidal V. Hemostatic embolization of renal artery pseudoaneurysm using absorbable surgical suture (FairEmbo Concept). Diagn Interv Imaging. 2020; Doi: https://doi.org/10.1016/j.diii.2020.04.002
Doucet J, Kiri L, O’Connell K, Kehoe S, Lewandowski R, Liu D, et al. Advances in degradable embolic microspheres: a state of the art review. J Funct Biomater. 2018;9(1):14. https://doi.org/10.3390/jfb9010014.
Li M. Progress in research and application of PLGA embolic microspheres. Front Biosci. 2016;21(5):931–40. https://doi.org/10.2741/4430.
Kucukay F, Topcuoglu OM, Alpar A, Altay ÇM, Kucukay MB, Ozbulbul NI. Bronchial artery embolization with large sized (700–900 µm) tris-acryl microspheres (embosphere) for massive hemoptysis: long-term results (clinical research). Cardiovasc Intervent Radiol. 2018;41(2):225–30. https://doi.org/10.1007/s00270-017-1818-7.
Chatziioannou A, Gargas D, Malagari K, Kornezos I, Ioannidis I, Primetis E, et al. Transcatheter arterial embolization as therapy of renal angiomyolipomas: the evolution in 15 years of experience. Eur J Radiol. 2012;81(9):2308–12. https://doi.org/10.1016/j.ejrad.2011.06.003.
Swindle MM, Makin A, Herron AJ, Clubb FJ, Frazier KS. Swine as models in biomedical research and toxicology testing. Vet Pathol. 2012;49(2):344–56. https://doi.org/10.1177/0300985811402846.
Pereira-Sampaio MA, Favorito LA, Sampaio FJB. Pig kidney: anatomical relationships between the intrarenal arteries and the kidney collecting system. applied study for urological research and surgical training. J Urol. 2004;172(5):2077–81. https://doi.org/10.1097/01.ju.0000138085.19352.b5.
Link DP, Strandberg JD, Virmani R, Blashka K, Mourtada F, Samphilipo MA. Histopathologic appearance of arterial occlusions with hydrogel and polyvinyl alcohol embolic material in domestic swine. J Vasc Interv Radiol. 1996;7(6):897–906. https://doi.org/10.1016/s1051-0443(96)70868-0.
Trerotola SO, Pressler GA, Premanandan C. Nylon fibered versus non-fibered embolization coils: comparison in a swine model. J Vasc Interv Radiol. 2019;30(6):949–55. https://doi.org/10.1016/j.jvir.2018.10.004.
Girdhar G, Read M, Sohn J, Shah C, Shrivastava S. In-vitro thrombogenicity assessment of polymer filament modified and native platinum embolic coils. J Neurol Sci. 2014;339(1–2):97–101. https://doi.org/10.1016/j.jns.2014.01.030.
Spies JB, Allison S, Flick P, McCullough M, Sterbis K, Cramp M, et al. Polyvinyl alcohol particles and tris-acryl gelatin microspheres for uterine artery embolization for leiomyomas: results of a randomized comparative study. J Vasc Interv Radiol. 2004;15(8):793–800. https://doi.org/10.1097/01.RVI.0000136982.42548.5D.
Falagas ME, Nikou SA, Siempos II. Infections related to coils used for embolization of arteries: review of the published evidence. J Vasc Interv Radiol. 2007;18(6):697–701. https://doi.org/10.1016/j.jvir.2007.04.015.
Vrachliotis TG, Falagas ME. Infections after endovascular coil embolization. J Endovascu Ther. 2007;14(6):805–6. https://doi.org/10.1583/07-2219C.1.
Lechner R, Helm M, Müller M, Wille T, Riesner HJ, Friemert B. In-vitro study of species-specific coagulation differences in animals and humans using rotational thromboelastometry (ROTEM). J R Army Med Corps. 2019;165(5):356–9. https://doi.org/10.1136/jramc-2018-001092.
Kessler U, Grau T, Gronchi F, Berger S, Brandt S, Bracht H, et al. Comparison of porcine and human coagulation by thrombelastometry. Thromb Res. 2011;128(5):477–82. https://doi.org/10.1016/j.thromres.2011.03.013.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Ethical Approval
All applicable international, national and/or institutional guidelines for the care and use of animals were conducted. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted (agreement of the Committee of Ethical Animal APAFIS#14851–2018042610172296).
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Bisceglie, M., Hak, JF., Diop, A.D. et al. FairEmbo Concept for Arterial Embolizations: In Vivo Feasibility and Safety Study with Suture-Based Microparticles Compared with Microspheres. Cardiovasc Intervent Radiol 44, 625–632 (2021). https://doi.org/10.1007/s00270-020-02678-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02678-0