Abstract
Purpose
To assess the effect of contralateral dependent position on procedures and complications of percutaneous computed tomography (CT)-guided core needle biopsy (PCT-CNB) for small (≤ 20 mm) lung lesions adjacent to the pericardium.
Materials and Methods
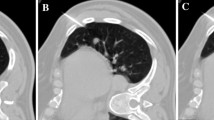
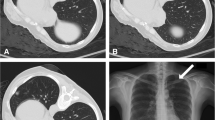
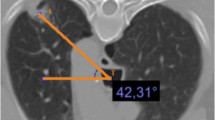
Retrospective view was performed to identify patients with small (≤ 20 mm) lung lesions located within 10 mm of the pericardium and who underwent PCT-CNB in the standard supine or prone position (n = 66) or in contralateral dependent position ( n = 35) between March 2010 and January 2020. In 35 patients, CT images in the contralateral dependent position were compared with images in the supine position to assess the mean distance of the lesion from the pericardium and the mean length of interface between these two positions. Complications including rates of pneumothorax, chest tube insertion, and pulmonary hemorrhage were assessed.
Results
In comparison with axial images in supine position, the pericardium were located farther from the lesion in the contralateral dependent position; the mean distance of lesions from the pericardium became farther (P < 0.001), and the mean length of interface with the pericardium became shorter (P = 0.008). There was no difference in the complication rates between supine or prone position and contralateral dependent position (pneumothorax, P = 0.098; pulmonary hemorrhage, P = 0.791).
Conclusion
Placing patients in contralateral dependent position may confer some advantages, including maximizing distance and minimizing length of interface of the lesion to the pericardium during PCT-CNB for small (≤ 20 mm) lung lesions adjacent to the pericardium.




Similar content being viewed by others
References
Henschke CI. Early lung cancer action project: overall design and findings from baseline screening. Cancer. 2000;89(11 Suppl):2474–82.
Diederich S, Wormanns D, Semik M, Thomas M, Lenzen H, Roos N, et al. Screening for early lung cancer with low-dose spiral CT: prevalence in 817 asymptomatic smokers. Radiology. 2002;222(3):773–81. https://doi.org/10.1148/radiol.2223010490.
Li Y, Du Y, Yang HF, Yu JH, Xu XX. CT-guided percutaneous core needle biopsy for small (</=20 mm) pulmonary lesions. Clin Radiol. 2013;68(1):e43–e4848. https://doi.org/10.1016/j.crad.2012.09.008.
Lee SM, Park CM, Lee KH, Bahn YE, Kim JI, Goo JM. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: clinical experience in 1108 patients. Radiology. 2014;271(1):291–300. https://doi.org/10.1148/radiol.13131265.
Wallace MJ, Krishnamurthy S, Broemeling LD, Gupta S, Ahrar K, Morello FA Jr, et al. CT-guided percutaneous fine-needle aspiration biopsy of small (< or =1-cm) pulmonary lesions. Radiology. 2002;225(3):823–8. https://doi.org/10.1148/radiol.2253011465.
Manhire A, Charig M, Clelland C, Gleeson F, Miller R, Moss H, et al. Guidelines for radiologically guided lung biopsy. Thorax. 2003;58(11):920–36.
Li C, Liu B, Meng H, Lv W, Jia H. Efficacy and radiation exposure of ultra-low-dose chest CT at 100 kVp with tin filtration in CT-guided percutaneous core needle biopsy for small pulmonary lesions using a third-generation dual-source CT scanner. J Vascular Interventional Radiol. 2019;30(1):95–102. https://doi.org/10.1016/j.jvir.2018.06.013.
Moore EH, Shepard JA, McLoud TC, Templeton PA, Kosiuk JP. Positional precautions in needle aspiration lung biopsy. Radiology. 1990;175(3):733–5. https://doi.org/10.1148/radiology.175.3.2343123.
Heerink WJ, de Bock GH, de Jonge GJ, Groen HJ, Vliegenthart R, Oudkerk M. Complication rates of CT-guided transthoracic lung biopsy: meta-analysis. Eur Radiol. 2017;27(1):138–48. https://doi.org/10.1007/s00330-016-4357-8.
Neyaz Z, Mohindra N. Is the rapid needle-out patient-rollover approach after CT-guided lung biopsy really effective for pneumothorax prevention? J Thoracic Disease. 2015;7(9):E350–E353353. https://doi.org/10.3978/j.issn.2072-1439.2015.09.34.
O'Neill AC, McCarthy C, Ridge CA, Mitchell P, Hanrahan E, Butler M, et al. Rapid needle-out patient-rollover time after percutaneous CT-guided transthoracic biopsy of lung nodules: effect on pneumothorax rate. Radiology. 2012;262(1):314–9. https://doi.org/10.1148/radiol.11103506.
Drumm O, Joyce EA, de Blacam C, Gleeson T, Kavanagh J, McCarthy E, et al. CT-guided lung biopsy: effect of biopsy-side down position on pneumothorax and chest tube placement. Radiology. 2019;292(1):190–6. https://doi.org/10.1148/radiol.2019182321.
Kim JI, Park CM, Lee SM, Goo JM. Rapid needle-out patient-rollover approach after cone beam CT-guided lung biopsy: effect on pneumothorax rate in 1,191 consecutive patients. Eur Radiol. 2015;25(7):1845–53. https://doi.org/10.1007/s00330-015-3601-y.
Hsu LS, Chen CW, Chang CH, Liao CH, Hsu SL, Lin WM. Influences of cardiac motion on computed tomography-guided biopsy of lung nodules located near the heart. Medicine. 2017;96(46):e8558. https://doi.org/10.1097/MD.0000000000008558.
Mu L, Pan T, Lyu N, Sun L, Li S, Xie Q, et al. CT-guided percutaneous radiofrequency ablation for lung neoplasms adjacent to the pericardium. Lung cancer. 2018;122:25–31. https://doi.org/10.1016/j.lungcan.2018.05.004.
Iguchi T, Hiraki T, Gobara H, Mimura H, Fujiwara H, Tajiri N, et al. Percutaneous radiofrequency ablation of lung tumors close to the heart or aorta: evaluation of safety and effectiveness. J Vascular Interventional Radiol 2007;18(6):733–40. https://doi.org/10.1016/j.jvir.2007.02.024.
Maxwell AWP, Healey TT, Dupuy DE. Microwave ablation of lung tumors near the heart: a retrospective review of short-term procedural safety in ten patients. Cardiovasc Intervent Radiol. 2017;40(9):1401–7. https://doi.org/10.1007/s00270-017-1660-y.
Yeow KM, Su IH, Pan KT, Tsay PK, Lui KW, Cheung YC, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004;126(3):748–54. https://doi.org/10.1378/chest.126.3.748.
Tai R, Dunne RM, Trotman-Dickenson B, Jacobson FL, Madan R, Kumamaru KK, et al. Frequency and severity of pulmonary hemorrhage in patients undergoing percutaneous CT-guided transthoracic lung biopsy: single-institution experience of 1175 cases. Radiology. 2016;279(1):287–96. https://doi.org/10.1148/radiol.2015150381.
Rebonato A, Maiettini D, Andolfi M, Fischer MJ, Vannucci J, Metro G, et al. CT-guided percutaneous trans-scapular lung biopsy in the diagnosis of peripheral pulmonary lesion nodules of the superior lobes using large needles. Cardiovasc Intervent Radiol. 2018;41(2):284–90. https://doi.org/10.1007/s00270-017-1768-0.
Chehab M, Zintsmaster S, Jafri SZ, Richards M, Roy A. CT-guided transosseous soft tissue biopsy: techniques, outcomes and complications in 50 cases. Cardiovasc Intervent Radiol. 2017;40(9):1461–8. https://doi.org/10.1007/s00270-017-1669-2.
Kucharczyk W, Weisbrod GL, Cooper JD, Todd T. Cardiac tamponade as a complication of thin-needle aspiration lung biopsy. Chest. 1982;82(1):120–1. https://doi.org/10.1378/chest.82.1.120.
Shevland JE. Right ventricular perforation: a rare complication of percutaneous lung biopsy. J Thorac Imaging. 1991;6(4):85–6.
Mitchell MJ, Montgomery M, Reiter CG, Culp WC Jr. Pericardial tamponade following CT-guided lung biopsy. Cardiovasc Intervent Radiol. 2008;31(Suppl 2):S227–S23030. https://doi.org/10.1007/s00270-007-9210-7.
Cheung YC, Chang JW, Hsieh JJ, Lin G, Tsai YH. Adequacy and complications of computed tomography-guided core needle biopsy on non-small cell lung cancers for epidermal growth factor receptor mutations demonstration: 18-gauge or 20-gauge biopsy needle. Lung cancer. 2010;67(2):166–9. https://doi.org/10.1016/j.lungcan.2009.04.007.
Ozturk K, Soylu E, Gokalp G, Topal U. Risk factors of pneumothorax and chest tube placement after computed tomography-guided core needle biopsy of lung lesions: a single-centre experience with 822 biopsies. Polish journal of radiology. 2018;83:e407–e414414. https://doi.org/10.5114/pjr.2018.79205.
Rozenblit AM, Tuvia J, Rozenblit GN, Klink A. CT-guided transthoracic needle biopsy using an ipsilateral dependent position. AJR Am J Roentgenol. 2000;174(6):1759–64. https://doi.org/10.2214/ajr.174.6.1741759.
Leger T, Jerjir N, Gregory J, Bennani S, Freche G, Revel MP, et al. Does Ipsilateral-Dependent Positioning During Percutaneous Lung Biopsy Decrease the Risk of Pneumothorax? AJR Am J Roentgenol. 2019;212(2):461–6. https://doi.org/10.2214/AJR.18.19871.
Wang Y, Li W, He X, Li G, Xu L. Computed tomography-guided core needle biopsy of lung lesions: diagnostic yield and correlation between factors and complications. Oncology letters. 2014;7(1):288–94. https://doi.org/10.3892/ol.2013.1680.
Yang W, Sun W, Li Q, Yao Y, Lv T, Zeng J, et al. Diagnostic accuracy of CT-guided transthoracic needle biopsy for solitary pulmonary nodules. PLoS ONE. 2015;10(6):e0131373. https://doi.org/10.1371/journal.pone.0131373.
Takeshita J, Masago K, Kato R, Hata A, Kaji R, Fujita S, et al. CT-guided fine-needle aspiration and core needle biopsies of pulmonary lesions: a single-center experience with 750 biopsies in Japan. AJR Am J Roentgenol. 2015;204(1):29–34. https://doi.org/10.2214/AJR.14.13151.
Mills M, Choi J, El-Haddad G, Sweeney J, Biebel B, Robinson L, et al. Retrospective analysis of technical success rate and procedure-related complications of 867 percutaneous CT-guided needle biopsies of lung lesions. Clin Radiol. 2017;72(12):1038–46. https://doi.org/10.1016/j.crad.2017.07.023.
Anzidei M, Sacconi B, Fraioli F, Saba L, Lucatelli P, Napoli A, et al. Development of a prediction model and risk score for procedure-related complications in patients undergoing percutaneous computed tomography-guided lung biopsy. Eur J Cardio-Thoracic Surg Official J Eur Assoc Cardio-thoracic Surg. 2015;48(1):e1–6. https://doi.org/10.1093/ejcts/ezv172.
Laurent F, Latrabe V, Vergier B, Montaudon M, Vernejoux JM, Dubrez J. CT-guided transthoracic needle biopsy of pulmonary nodules smaller than 20 mm: results with an automated 20-gauge coaxial cutting needle. Clin Radiol. 2000;55(4):281–7. https://doi.org/10.1053/crad.1999.0368.
Nour-Eldin NE, Alsubhi M, Naguib NN, Lehnert T, Emam A, Beeres M, et al. Risk factor analysis of pulmonary hemorrhage complicating CT-guided lung biopsy in coaxial and non-coaxial core biopsy techniques in 650 patients. Eur J Radiol. 2014;83(10):1945–52. https://doi.org/10.1016/j.ejrad.2014.06.023.
Acknowledgment
None.
Funding
This study was funded by National Key Research and Development Programe of China (No. 2016YFC0106203) and Programe of Shanghai Hospital Development Center (No. SHDC22017102).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
For retrospective studies, formal consent is not required.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, C., Xu, L., He, J. et al. Contralateral Dependent Position During Percutaneous CT-Guided Core Needle Biopsy for Small (≤ 20 mm) Lung Lesions Adjacent to the Pericardium: Effect on Procedures and Complications. Cardiovasc Intervent Radiol 43, 1652–1660 (2020). https://doi.org/10.1007/s00270-020-02608-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-020-02608-0