Abstract
Purpose
Patients with hepatocellular carcinoma and portal vein tumor thrombus have a poor prognosis and limited therapeutic options. We sought to compare survival, tolerability, and safety in such patients treated with conventional yttrium-90 transarterial radioembolization dosimetric techniques or ablative transarterial radioembolization.
Materials and Methods
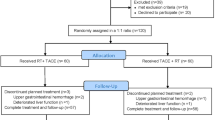
This retrospective, single-center cohort study included patients with hepatocellular carcinoma and right, left, and/or main portal vein tumor thrombus, preserved liver function (Child–Pugh class ≤ B7), and good performance status (Eastern Cooperative Oncology Group score ≤ 1) treated with yttrium-90 microspheres from 2011 to 2018 with ablative intent transarterial radioembolization (A-TARE), or conventional technique (cTARE). Statistical models were used to compare overall survival, post-treatment survival, toxicities, and prognosticators of response.
Results
Fifty-seven patients were included (21 [36.8%] ablative and 36 [63.2%] conventional intent). Median overall survival was 15.7 months. Compared to conventional treatment, ablative radioembolization was associated with longer median overall survival (45.3 vs 18.2 months; P = 0.003), longer post-treatment survival (19.1 vs 4.9 months; P = 0.005), a 70% lower risk of death (hazard ratio 0.30; 95% confidence interval, 0.13–0.70; P = 0.005), and improved 4-year survival (53.9% vs 11.2%). Overall survival did not differ significantly between treatment with resin and glass microspheres (27.5 vs 22.2 months; P = 0.62). Acceptable hepatic toxicities were observed after yttrium-90 administration, without statistical differences between the groups.
Conclusion
In patients with advanced hepatocellular carcinoma and portal vein tumor thrombus, A-TARE is associated with longer survival than cTARE. Neither modality is associated with deleterious effects on liver function.




Similar content being viewed by others
References
Titano J, Noor A, Kim E. Transarterial chemoembolization and radioembolization across barcelona clinic liver cancer stages. Semin Intervent Radiol. 2017;34:109–15.
Han K, Kim JH, Ko GY, Gwon DI, Sung KB. Treatment of hepatocellular carcinoma with portal venous tumor thrombosis: a comprehensive review. World J Gastroenterol. 2016;22:407–16.
Yu SJ, Kim YJ. Effective treatment strategies other than sorafenib for the patients with advanced hepatocellular carcinoma invading portal vein. World J Hepatol. 2015;7:1553–61.
Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999;29:62–7.
Minagawa M, Makuuchi M. Treatment of hepatocellular carcinoma accompanied by portal vein tumor thrombus. World J Gastroenterol. 2006;12:7561–7.
Schoniger-Hekele M, Muller C, Kutilek M, Oesterreicher C, Ferenci P, Gangl A. Hepatocellular carcinoma in Central Europe: prognostic features and survival. Gut. 2001;48:103–9.
Chow PKH, Gandhi M, Tan SB, Khin MW, Khasbazar A, Ong J, et al. SIRveNIB: selective internal radiation therapy versus sorafenib in Asia-Pacific patients with hepatocellular carcinoma. J Clin Oncol. 2018;36:1913–21.
Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378–90.
Vilgrain V, Pereira H, Assenat E, Guiu B, Ilonca AD, Pageaux GP, et al. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. Lancet Oncol. 2017;18:1624–36.
Yoon SM, Ryoo BY, Lee SJ, Kim JH, Shin JH, An JH, et al. Efficacy and safety of transarterial chemoembolization plus external beam radiotherapy versus sorafenib in hepatocellular carcinoma with macroscopic vascular invasion: a randomized clinical trial. JAMA Oncol. 2018;4:661–9.
Gbolahan OB, Schacht MA, Beckley EW, LaRoche TP, O’Neil BH, Pyko M. Locoregional and systemic therapy for hepatocellular carcinoma. J Gastrointest Oncol. 2017;8:215–28.
Li C, Hu J, Zhou D, Zhao J, Ma K, Yin X, et al. Differentiation of bland from neoplastic thrombus of the portal vein in patients with hepatocellular carcinoma: application of susceptibility-weighted MR imaging. BMC Cancer. 2014;14:590.
Lau WY, Kennedy AS, Kim YH, Lai HK, Lee RC, Leung TW, et al. Patient selection and activity planning guide for selective internal radiotherapy with yttrium-90 resin microspheres. Int J Radiat Oncol Biol Phys. 2012;82:401–7.
Lewandowski RJ, Gabr A, Abouchaleh N, Ali R, Al Asadi A, Mora RA, et al. Radiation segmentectomy: potential curative therapy for early hepatocellular carcinoma. Radiology. 2018;287:1050–8.
Riaz A, Gates VL, Atassi B, Lewandowski RJ, Mulcahy MF, Ryu RK, et al. Radiation segmentectomy: a novel approach to increase safety and efficacy of radioembolization. Int J Radiat Oncol Biol Phys. 2011;79:163–71.
Kallini JR, Gabr A, Salem R, Lewandowski RJ. Transarterial radioembolization with yttrium-90 for the treatment of hepatocellular carcinoma. Adv Ther. 2016;33:699–714.
Theysohn JM, Ertle J, Müller S, Schlaak JF, Nensa F, Sipilae S, et al. Hepatic volume changes after lobar selective internal radiation therapy (SIRT) of hepatocellular carcinoma. Clin Radiol. 2014;69:172–8.
Vouche M, Habib A, Ward TJ, Kim E, Kulik L, Ganger D, et al. Unresectable solitary hepatocellular carcinoma not amenable to radiofrequency ablation: multicenter radiology-pathology correlation and survival of radiation segmentectomy. Hepatology. 2014;60:192–201.
Vouche M, Lewandowski RJ, Atassi R, Memon K, Gates VL, Ryu RK, et al. Radiation lobectomy: time-dependent analysis of future liver remnant volume in unresectable liver cancer as a bridge to resection. J Hepatol. 2013;59:1029–36.
Padia SA, Johnson GE, Horton KJ, Ingraham CR, Kogut MJ, Kwan S, et al. Segmental yttrium-90 radioembolization versus segmental chemoembolization for localized hepatocellular carcinoma: results of a single-center, retrospective, propensity score-matched study. J Vasc Interv Radiol. 2017;28(777–785):e771.
Padia SA, Kwan SW, Roudsari B, Monsky WL, Coveler A, Harris WP. Superselective yttrium-90 radioembolization for hepatocellular carcinoma yields high response rates with minimal toxicity. J Vasc Interv Radiol. 2014;25:1067–73.
Ng E, Chung J, Klass D, Ho S, Patel R, Chou F, et al. Optimized computed tomographic angiography vessel evaluation protocol (OCTAVE) prior to transarterial radioembolization. Intervent Oncol. 2016;360(11):E183–93.
Gaba RC, Lewandowski RJ, Hickey R, Baerlocher MO, Cohen EI, Dariushnia SR, et al. Transcatheter therapy for hepatic malignancy: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2016;27:457–73.
Kennedy A, Nag S, Salem R, Murthy R, McEwan AJ, Nutting C, et al. Recommendations for radioembolization of hepatic malignancies using yttrium-90 microsphere brachytherapy: a consensus panel report from the radioembolization brachytherapy oncology consortium. Int J Radiat Oncol Biol Phys. 2007;68:13–23.
Padia SA, Lewandowski RJ, Johnson GE, Sze DY, Ward TJ, Gaba RC, et al. Radioembolization of hepatic malignancies: background, quality improvement guidelines, and future directions. J Vasc Interv Radiol. 2017;28:1–15.
Biederman DM, Titano JJ, Korff RA, Fischman AM, Patel RS, Nowakowski FS, et al. Radiation segmentectomy versus selective chemoembolization in the treatment of early-stage hepatocellular carcinoma. J Vasc Interv Radiol. 2018;29(30–37):e32.
Gulec SA, Mesoloras G, Stabin M. Dosimetric techniques in 90Y-microsphere therapy of liver cancer: the MIRD equations for dose calculations. J Nucl Med. 2006;47:1209–11.
Ho S, Lau WY, Leung TW, Chan M, Ngar YK, Johnson PJ, et al. Partition model for estimating radiation doses from yttrium-90 microspheres in treating hepatic tumours. Eur J Nucl Med. 1996;23:947–52.
Woo HY, Heo J. New perspectives on the management of hepatocellular carcinoma with portal vein thrombosis. Clin Mol Hepatol. 2015;21:115–21.
Abouchaleh N, Gabr A, Ali R, Al Asadi A, Mora RA, Kallini JR, et al. 90Y radioembolization for locally advanced hepatocellular carcinoma with portal vein thrombosis: long-term outcomes in a 185-patient cohort. J Nucl Med. 2018;59:1042–8.
Biederman DM, Titano JJ, Tabori NE, Pierobon ES, Alshebeeb K, Schwartz M, et al. Outcomes of radioembolization in the treatment of hepatocellular carcinoma with portal vein invasion: resin versus glass microspheres. J Vasc Interv Radiol. 2016;27(812–821):e812.
Floridi C, Pesapane F, Angileri SA, De Palma D, Fontana F, Caspani F, et al. Yttrium-90 radioembolization treatment for unresectable hepatocellular carcinoma: a single-centre prognostic factors analysis. Med Oncol. 2017;34:174.
Golfieri R, Mosconi C, Cappelli A, Giampalma E, Galaverni MC, Pettinato C, et al. Efficacy of radioembolization according to tumor morphology and portal vein thrombosis in intermediate-advanced hepatocellular carcinoma. Future Oncol. 2015;11:3133–42.
Kulik LM, Carr BI, Mulcahy MF, Lewandowski RJ, Atassi B, Ryu RK, et al. Safety and efficacy of 90Y radiotherapy for hepatocellular carcinoma with and without portal vein thrombosis. Hepatology. 2008;47:71–81.
Memon K, Kulik L, Lewandowski RJ, Mulcahy MF, Benson AB, Ganger D, et al. Radioembolization for hepatocellular carcinoma with portal vein thrombosis: impact of liver function on systemic treatment options at disease progression. J Hepatol. 2013;58:73–80.
Salem R, Lewandowski RJ, Mulcahy MF, Riaz A, Ryu RK, Ibrahim S, et al. Radioembolization for hepatocellular carcinoma using yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology. 2010;138:52–64.
Tsai AL, Burke CT, Kennedy AS, Moore DT, Mauro MA, Dixon RD, et al. Use of yttrium-90 microspheres in patients with advanced hepatocellular carcinoma and portal vein thrombosis. J Vasc Interv Radiol. 2010;21:1377–84.
Van Der Gucht A, Jreige M, Denys A, Blanc-Durand P, Boubaker A, Pomoni A, et al. Resin versus glass microspheres for (90)Y transarterial radioembolization: comparing survival in unresectable hepatocellular carcinoma using pretreatment partition model dosimetry. J Nucl Med. 2017;58:1334–40.
Boas FE, Bodei L, Sofocleous CT. Radioembolization of colorectal liver metastases: indications, technique, and outcomes. J Nucl Med. 2017;58:104S–11S.
Cremonesi M, Chiesa C, Strigari L, Ferrari M, Botta F, Guerriero F, et al. Radioembolization of hepatic lesions from a radiobiology and dosimetric perspective. Front Oncol. 2014;4:210.
Kokabi N, Camacho JC, Xing M, El-Rayes BF, Spivey JR, Knechtle SJ, et al. Open-label prospective study of the safety and efficacy of glass-based yttrium-90 radioembolization for infiltrative hepatocellular carcinoma with portal vein thrombosis. Cancer. 2015;121:2164–74.
Salem R, Thurston KG. Radioembolization with 90Y microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies. Part 1: technical and methodologic considerations. J Vasc Interv Radiol. 2006;17:1251–78.
Abi-Jaoudeh N. Resin versus glass microspheres. J Vasc Interv Radiol. 2016;27:822–3.
Ahmadzadehfar H, Meyer C, Pieper CC, Bundschuh R, Muckle M, Gartner F, et al. Evaluation of the delivered activity of yttrium-90 resin microspheres using sterile water and 5% glucose during administration. EJNMMI Res. 2015;5:54.
Westcott MA, Coldwell DM, Liu DM, Zikria JF. The development, commercialization, and clinical context of yttrium-90 radiolabeled resin and glass microspheres. Adv Radiat Oncol. 2016;1:351–64.
Gaba RC, Lewandowski RJ, Kulik LM, Riaz A, Ibrahim SM, Mulcahy MF, et al. Radiation lobectomy: preliminary findings of hepatic volumetric response to lobar yttrium-90 radioembolization. Ann Surg Oncol. 2009;16:1587–96.
Jakobs TF, Saleem S, Atassi B, et al. Fibrosis, portal hypertension, and hepatic volume. changes induced by intra-arterial radiotherapy with yttrium-90 microspheres. Dig Dis Sci. 2008;53:2556–63.
Chou WC, Lee CL, Yang TS, Huang CY, Teng W, Tseng YT, et al. Changes in serum α-fetoprotein level predicts treatment response and survival in hepatocellular carcinoma patients and literature review. J Formos Med Assoc. 2018;117:153–63.
Acknowledgements
The authors thank Ashley McCrea-Strub, PhD for performing statistical analyses and Sara Gardenghi, PhD; Chantal Caviness, MD, MPH, PhD; Kristina Wasson-Blader, PhD, ELS; Shannon Hach, MD, ELS; Adia Shy, PhD; and Edward Gloria of Eubio for editorial support. D.K. has received personal fees from Merit Medical, Cook Medical, LivaNova, Surefire Medical, Philips Healthcare, grants from Biolife, outside the submitted work. H.L. has received personal fees from Roche, Ipsen, Eisai, Taiho, Lilly, and LEO, outside the submitted work. D.M.L. has received grants and personal fees from Sirtex Medical, Grants and personal fees from BTG, outside the submitted work.
Funding
This study was not supported by any funding. Medical writing support was funded by Sirtex Medical, Inc., and performed by Eubio LLC.
Author information
Authors and Affiliations
Contributions
LCL, JC, DK, SH, AH, and DML developed the concept and designed the study, acquired and analyzed the data, and interpreted and discussed the results. LCL, VM, HL, AH, PK, and DML participated in drafting the manuscript and critically revised its intellectual content. All authors approved the final version of the manuscript. All authors agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare that they have no conflict of interest.
Consent for Publication
For this type of study consent for publication is not required.
Ethical Approval
For this type of study formal consent is not required. The study was approved by the institutional review board.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cardarelli-Leite, L., Chung, J., Klass, D. et al. Ablative Transarterial Radioembolization Improves Survival in Patients with HCC and Portal Vein Tumor Thrombus. Cardiovasc Intervent Radiol 43, 411–422 (2020). https://doi.org/10.1007/s00270-019-02404-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-019-02404-5