Abstract
Purpose
To evaluate the outcomes of fenestrated thoracic endovascular aortic repair (f-TEVAR) using physician-modified stent grafts (PMSGs) in zone 0 and zone 1 for aortic arch diseases.
Methods
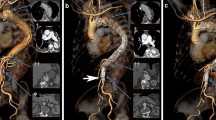
f-TEVAR using PMSGs in Z0 and Z1 was performed on ten high-risk patients for open surgery from November 2015 to September 2017. Indications were complicated acute type B dissection (ABAD) with retrograde dissection involving the mid-arch (n = 1), distal arch aneurysms (n = 3), mid-arch aneurysms of the inner arch curvature (n = 3) and penetrating aortic ulcer located in the mid- or proximal arch (n = 3). Pre-, intra- and postoperative clinical data were recorded.
Results
The median patient age was 61 (range 45–81) years, and 9 (90%) patients were men. Ten PMSGs (Medtronic Valiant stent grafts, n = 1; Relay thoracic stent grafts, n = 4; Cook TX2 device, n = 5) were deployed. PMSGs were deployed from Z0 and Z1 in 5 and 5 patients, respectively. Double small fenestrations for the left subclavian artery (LSA) and the left common carotid artery (LCCA), respectively, were created in 3 patients. Triple small fenestrations for the innominate artery (IA), the LCCA and the LSA, respectively, were created in 2 patients. One large fenestration for both the IA and the LCCA combined with one small fenestration for the LSA was created in 3 patients. One large fenestration for the LCCA combined with one small fenestration for the LSA was created in 2 patients. Posterior diameter-reducing ties were added to all the devices except to one Valiant stent graft. All but 2 patients underwent elective procedure. Median duration for stent graft modifications was 105 (range 90–125) min. The technical success rate was 90%. Overall mortality was 10% (1/10). One patient died of sudden cardiac arrest intraoperatively after the deployment of the PMSG and all the supra-aortic branch stents. Mean operative time was 106.0 ± 43.0 min, and fluoroscopy time was 30.6 ± 22.9 min. There were no type I or type III endoleaks, perioperative neurological complications or spinal cord ischemia. Median length of stay was 8 (range 4–35) days. Nine patients survived at mean 13.3 (range 6.0–19.0) months follow-up. Retrograde dissection occurred in one patient of Z0 group 40 days post-f-TEVAR and resolved after open repair. During follow-up, all target vessels remained patent without fenestration-related type I or III endoleaks.
Conclusions
f-TEVAR using PMSGs in Z0 and Z1 for the treatment of aortic arch diseases in high-risk patients is feasible in the hands of experienced operators.




Similar content being viewed by others
Abbreviations
- f-TEVAR:
-
Fenestrated thoracic endovascular aortic repair
- PMSG:
-
Physician-modified stent graft
- ABAD:
-
Acute type B dissection
- CTA:
-
Computed tomography angiography
- IA:
-
Innominate artery
- LCCA:
-
Left common carotid artery
- LSA:
-
Left subclavian artery
- ASA:
-
American Society of Anesthesiologists
- RTAD:
-
Retrograde type A aortic dissections
- RAO:
-
Right anterior oblique
- LAO:
-
Left anterior oblique
References
Estrera AL, Miller CC 3rd, Lee TY, Shah P, Safi HJ. Ascending and transverse aortic arch repair: the impact of retrograde cerebral perfusion. Circulation. 2008;118(Suppl):S160–6.
Riambau V, Böckler D, Brunkwall J, Cao P, Chiesa R, Coppi G, et al. Editor’s choice-management of descending thoracic aorta diseases: clinical practice guidelines of the European society for vascular surgery (ESVS). Eur J Vasc Endovasc Surg. 2017;53(1):4–52.
Redlinger RE Jr, Ahanchi SS, Panneton JM. In situ laser fenestration during emergent thoracic endovascular aortic repair is an effective method for left subclavian artery revascularization. J Vasc Surg. 2013;58(5):1171–7.
Wang T, Shu C, Li QM, Li M, Li X, He H, et al. First experience with the double chimney technique in the treatment of aortic arch diseases. J Vasc Surg. 2017;66(4):1018–27.
Kurimoto Y, Maruyama R, Ujihira K, Nishioka N, Hasegawa K, Iba Y, et al. Thoracic endovascular aortic repair for challenging aortic arch diseases using fenestrated stent grafts from zone 0. Ann Thorac Surg. 2015;100(1):24–32 discussion 32–33.
Zhu J, Zhao L, Dai X, Luo Y, Fan H, Feng Z, Zhang Y, Hu F. Fenestrated thoracic endovascular aortic repair using physician modified stent grafts for acute type B aortic dissection with unfavourable landing zone. Eur J Vasc Endovasc Surg. 2018;55(2):170–6.
Oderich GS. Technique of adding a diameter-reducing wire to the modified TX2 fenestrated stent graft. Vascular. 2010;18(6):350–5.
Iba Y, Minatoya K, Matsuda H, Sasaki H, Tanaka H, Kobayashi J, et al. Contemporary open aortic arch repair with selective cerebral perfusion in the era of endovascular aortic repair. J Thorac Cardiovasc Surg. 2013;145(3 Suppl):S72–7.
Kurazumi H, Mikamo A, Kudo T, Suzuki R, Takahashi M, Shirasawa B, et al. Aortic arch surgery in octogenarians: is it justified? Eur J Cardiothorac Surg. 2014;46(4):672–7.
Geisbüsch P, Kotelis D, Müller-Eschner M, Hyhlik-Dürr A, Böckler D. Complications after aortic arch hybrid repair. J Vasc Surg. 2011;53(4):935–41.
Spanos K, Tsilimparis N, Rohlffs F, Wipper S, Detter C, Behrendt CA, et al. Total endovascular arch repair is the procedure of the future. Part I. J Cardiovasc Surg (Torino). 2018. https://doi.org/10.23736/s0021-9509.18.10412-5 Epub ahead of print.
Cochennec F, Kobeiter H, Gohel M, Leopardi M, Raux M, Majewski M, et al. Early results of physician modified fenestrated stent grafts for the treatment of thoraco-abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2015;50(5):583–92.
Haulon S, Greenberg RK, Spear R, Eagleton M, Abraham C, Lioupis C, et al. Global experience with an inner branched arch endograft. J Thorac Cardiovasc Surg. 2014;148(4):1709–16.
Tsilimparis N, Debus ES, von Kodolitsch Y, Wipper S, Rohlffs F, Detter C, et al. Branched versus fenestrated endografts for endovascular repair of aortic arch lesions. J Vasc Surg. 2016;64(3):592–9.
Iwakoshi S, Ichihashi S, Itoh H, Tabayashi N, Sakaguchi S, Yoshida T, et al. Clinical outcomes of thoracic endovascular aneurysm repair using commercially available fenestrated stent graft (Najuta endograft). J Vasc Surg. 2015;62(6):1473–8.
Joseph G, Premkumar P, Thomson V, Varghese M, Selvaraj D, Sahajanandan R. Externalized guidewires to facilitate fenestrated endograft deployment in the Aortic Arch. J Endovasc Ther. 2016;23(1):160–71.
Tshomba Y, Bertoglio L, Marone EM, Logaldo D, Maisano F, Chiesa R. Retrograde type A dissection after endovascular repair of a “zone 0” nondissecting aortic arch aneurysm. Ann Vasc Surg. 2010;24(952):e1–7.
Preventza O, Garcia A, Moeller K, Cooley DA, Gonzalez L, Cheong BY, et al. Retrograde ascending aortic dissection after thoracic endovascular aortic repair for distal aortic dissection or with zone 0 landing: association, risk factors, and true incidence. Ann Thorac Surg. 2015;100(2):509–15.
Czerny M, Weigang E, Sodeck G, Schmidli J, Antona C, Gelpi G, et al. Targeting landing zone 0 by total arch rerouting and TEVAR: midterm results of a transcontinental registry. Ann Thorac Surg. 2012;94:84–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Rights and permissions
About this article
Cite this article
Zhu, J., Dai, X., Noiniyom, P. et al. Fenestrated Thoracic Endovascular Aortic Repair Using Physician-Modified Stent Grafts (PMSGs) in Zone 0 and Zone 1 for Aortic Arch Diseases. Cardiovasc Intervent Radiol 42, 19–27 (2019). https://doi.org/10.1007/s00270-018-2079-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2079-9