Abstract
Purpose
To identify baseline characteristics and long-term prognostic factors in non-transplant patients with unresectable hepatocellular carcinoma (HCC) who had prolonged survival after treatment with yttrium-90 radioembolization (Y90).
Materials and Methods
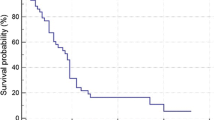
Sixty-seven “Super Survivors” (defined as ≥ 3-year survival after Y90) were identified within our 1000-patient Y90 database (2003–2017). Baseline imaging and follow-up occurred at 1 month and every 3 months thereafter. Overall survival (OS) was calculated with Kaplan–Meier estimates with log-rank test in subgroups: Child–Pugh (CP) score, distribution of disease, portal vein thrombus (PVT), and technique (segmental vs lobar Y90).
Results
Median age 69.5 years (range 45–94 years); 69% male; 60% solitary HCC; 79% unilobar disease; 12% PVT; 10% ascites; Barcelona Clinic Liver Cancer Stage A—54%/B—28%/C—16%/D—2%; CP A—70%/B—28%/C—2%. Longest baseline tumor diameter was 5.4 ± 4.0 cm (mean ± SD). All patients had an imaging response (either partial or complete response). Median OS was 67.5 months (95% CI 55.2–82.5). CP score and main PVT stratified median OS (p = 0.0007 and p = 0.0187, respectively). Beyond 3 years, segmental versus lobar Y90 was associated with improved OS with a median OS of 80.2 versus 46.7 months, respectively (p = 0.0024). Dosing > 200 Gy was not a significant predictor of improved OS.
Conclusions
Super Survivors spanning the BCLC staging system maintained durable OS after radioembolization that was stratified by the extent of underlying liver disease. The common variable among all patients was an imaging response. Segmental versus lobar Y90 may have a long-term associated OS benefit.


Similar content being viewed by others
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- AFP:
-
Alpha-Fetoprotein
- ALBI:
-
Albumin–bilirubin
- ALT:
-
ALanine transaminase
- AST:
-
ASpartate transaminase
- BCLC:
-
Barcelona Clinic Liver Cancer
- CI:
-
Confidence interval
- CR:
-
Complete response
- ECOG:
-
Eastern Cooperative Oncology Group
- EASL:
-
European Association for the Study of the Liver
- ESL:
-
Extended shelf life
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- IQR:
-
interquartile range
- KM:
-
Kaplan–Meier
- NASH:
-
Non-alcoholic steatohepatitis
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PVT:
-
Portal vein thrombosis
- PR:
-
Partial response
- RFA:
-
Radio frequency ablation
- SD:
-
Stable disease
- TACE:
-
TransArterial ChemoEmbolization
- TTP:
-
Time to progression
- WHO:
-
World Health Organization
- Y90:
-
Yttrium-90 radioembolization
References
Mazzaferro V, Sposito C, Bhoori S, Romito R, Chiesa C, Morosi C, et al. Yttrium-90 radioembolization for intermediate-advanced hepatocellular carcinoma: a phase 2 study. Hepatology. 2012;57:1826–37.
Kulik LM, Carr BI, Mulcahy MF, Lewandowski RJ, Atassi B, Ryu RK, et al. Safety and efficacy of 90Y radiotherapy for hepatocellular carcinoma with and without portal vein thrombosis. Hepatology. 2008;47:71–81.
Sangro B, Carpanese L, Cianni R, Golfieri R, Gasparini D, Ezziddin S, et al. Survival after yttrium-90 resin microsphere radioembolization of hepatocellular carcinoma across Barcelona Clinic Liver Cancer Stages: a European evaluation. Hepatology. 2011;54:868–78.
Salem R, Gabr A, Riaz A, Mora R, Ali R, Abecassis M, et al. Institutional decision to adopt Y90 as primary treatment for hepatocellular carcinoma informed by a 1000-patient 15-year experience. Hepatology. 2018. https://doi.org/10.1002/hep.29691.
Burrel M, Reig M, Forner A, Barrufet M, de Lope CR, Tremosini S, et al. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using drug eluting beads. Implications for clinical practice and trial design. J Hepatol. 2012;56:1330–5.
Vouche M, Habib A, Ward TJ, Kim E, Kulik L, Ganger D, et al. Unresectable solitary hepatocellular carcinoma not amenable to radiofrequency ablation: multicenter radiology-pathology correlation and survival of radiation segmentectomy. Hepatology. 2014;60:192–201.
Bruix J, Sherman M, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):102–1022.
Salem R, Lewandowski RJ, Gates VL, Nutting CW, Murthy R, Rose SC, et al. Research reporting standards for radioembolization of hepatic malignancies. J Vasc Interv Radiol. 2011;22(3):265–78.
Salem R, Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Ibrahim S, et al. Technical aspects of radioembolization with 90Y microspheres. Tech Vasc Interv Radiol. 2007;10:12–29.
Lewandowski RJ, Sato KT, Atassi B, Ryu RK, Nemcek AA Jr, Kulik L, et al. Radioembolization with 90Y microspheres: angiographic and technical considerations. Cardiovasc Inter Rad. 2007;30:571–92.
Riaz A, Gates VL, Atassi B, Lewandowski RJ, Mulcahy MF, Ryu RK, et al. Radiation segmentectomy: a novel approach to increase safety and efficacy of radioembolization. Int J Radiat Oncol Biol Phys. 2011;79:163–71.
Lewandowski RJ, Minocha J, Memon K, Riaz A. Sustained safety and efficacy of extended-shelf-life 90Y glass microspheres: long-term follow-up in a 134-patient cohort. Eur J Nucl Med Mol Imaging. 2014;41:486–93.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–16.
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35:421–30.
Riaz A, Miller FH, Kulik LM, Nikolaidis P, Yaghmai V, Lewandowski RJ, et al. Imaging response in the primary index lesion and clinical outcomes following transarterial locoregional therapy for hepatocellular carcinoma. JAMA. 2010;303:1062–9.
Biederman DM, Posham R, Durrani RJ, Titano JJ, Patel RS, Tabori NE, et al. Outcomes of radioembolization for unresectable hepatocellular carcinoma in patients with marginal functional hepatic reserve. Clin Imaging. 2018;47:34–40.
Riaz A, Gabr A, Abouchaleh N, Ali R, Asadi Al A, Mora R, et al. Radioembolization for hepatocellular carcinoma: statistical confirmation of improved survival in responders by landmark analyses. Hepatology. 2018;27:1485.
Garin E, Lenoir L, Edeline J, Laffont S, Mesbah H, Poree P, et al. Boosted selective internal radiation therapy with 90Y-loaded glass microspheres (B-SIRT) for hepatocellular carcinoma patients: a new personalized promising concept. Eur J Nucl Med Mol Imaging. 2013;40:1057–68.
Garin E, Rolland Y, Laffont S, Edeline J. Clinical impact of (99 m)Tc-MAA SPECT/CT-based dosimetry in the radioembolization of liver malignancies with (90)Y-loaded microspheres. Eur J Nucl Med Mol Imaging. 2016;43:559–75.
Srinivas SM, Natarajan N, Kuroiwa J, Gallagher S, Nasr E, Shah SN, et al. Determination of radiation absorbed dose to primary liver tumors and normal liver tissue using post-radioembolization (90)Y PET. Front Oncol. 2014;4:1–12.
Goin JE, Salem R, Carr BI, Dancey JE, Soulen MC, Geschwind J, et al. Treatment of unresectable hepatocellular carcinoma with intrahepatic yttrium 90 microspheres: factors associated with liver toxicities. JVIR. 2005;16:205–13.
Ahmed AF, Samreen N, Grajo JR, Zendejas I, Sistrom CL, Collinsworth A, et al. Angiosomal radiopathologic analysis of transarterial radioembolization for the treatment of hepatocellular carcinoma. Abdom Radiol. 2017;55:1197–209.
Salem R, Gordon AC, Mouli S, Hickey R, Kallini J, Gabr A, et al. Y90 radioembolization significantly prolongs time to progression compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2016;151:1155.e2–1163.e2.
Gabr A, Abouchaleh N, Ali R, Vouche M, Atassi R, Memon K, et al. Comparative study of post-transplant outcomes in hepatocellular carcinoma patients treated with chemoembolization or radioembolization. Eur J Radiol. 2017;93:100–6.
Prentice, MA. Changes to HCC criteria for auto approval. OPTN/UNOS Liver and Intestinal Organ Transplantation Committee. 2016. Retrieved from https://optn.transplant.hrsa.gov/governance/public-comment/hcc-auto-approval-criteria-changes/.
Massie AB, Caffo B, Gentry SE, Hall EC, Axelrod DA, Lentine KL, et al. MELD exceptions and rates of waiting list outcomes. Am J Transplant. 2011;11:2362–71.
Heimbach JK, Hirose R, Stock PG, Schladt DP, Xiong H, Liu J, et al. Delayed hepatocellular carcinoma model for end-stage liver disease exception score improves disparity in access to liver transplant in the United States. Hepatology. 2015;61:1643–50.
Acknowledgements
The authors thank Carlene del Castillo, Karen Grace, Krystina Salzig, and Melissa Williams for their commitment to patient care and dedication to clinical research.
Funding
ACG is a Medical Scientist Training Program student (T32GM008152).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RJL and RS serve as advisors to BTG. None of the other authors report a conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gordon, A.C., Gabr, A., Riaz, A. et al. Radioembolization Super Survivors: Extended Survival in Non-operative Hepatocellular Carcinoma. Cardiovasc Intervent Radiol 41, 1557–1565 (2018). https://doi.org/10.1007/s00270-018-2008-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2008-y