Abstract
Purpose
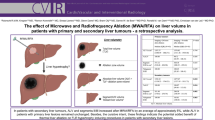
The “oven effect” theory assumes that radiofrequency ablation (RFA) would be more efficient on tumors of cirrhotic livers. The aim of the study was to compare the size and volume of the ablation zone following RFA on tumors of cirrhotic versus healthy livers.
Methods
One hundred and eleven patients who underwent RFA from 2011 to 2013 for the treatment of 140 liver tumors (83 hepatocellular carcinomas developed on a cirrhotic liver, i.e., “cirrhosis group,” and 57 tumors developed on a healthy liver, mainly liver metastasis, i.e., “healthy liver group”) using the same RFA device were retrospectively selected. The diameter and volume of the ablation zone were compared between groups at the end of the procedure (FU0), at first (FU1) and second follow-up (FU2) performed 1.6 months (± 19 days) and 4.7 months (± 40 days) post-RFA, respectively.
Results
No differences in the size or volume of the ablation zone were found between groups at FU0 (36.5 ± 12 mm vs. 34.3 ± 10 mm, p = 0.5; and 28 ± 16 mm3 vs. 26.5 ± 16 mm3, p = 0.6, respectively), FU1, or FU2. Similarly, no differences were found at FU0, FU1, or FU2 in the subgroups of tumors treated using a single radiofrequency application. The mean volume of the ablation zone decreased over time, by 33.3% at FU1 and 48.5% at FU2, without any difference between groups.
Conclusion
In contradiction to the “oven effect” theory, RFA achieves ablation zones of a comparable size and volume in cirrhotic and healthy livers.

Similar content being viewed by others
Abbreviations
- RFA:
-
Radiofrequency ablation
- HCC:
-
Hepatocellular carcinoma
- LM:
-
Liver metastasis
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- ALP:
-
Alkaline phosphatase
- GGT:
-
Gamma-glutamyl transferase
- PT:
-
Prothrombin time
References
Buscarini E, Savoia A, Brambilla G, et al. Radio frequency thermal ablation of liver tumors. Eur Radiol. 2005;15:884–94.
European Association For The Study Of The L, European Organisation For R, Treatment Of C. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–43.
Bruix J, Sherman M, American Association for the Study of Liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2.
Fang Y, Chen W, Liang X, et al. Comparison of long-term effectiveness and complications of radiofrequency ablation with hepatectomy for small hepatocellular carcinoma. J Gastroenterol Hepatol. 2014;29:193–200.
Cho YK, Kim JK, Kim MY, Rhim H, Han JK. Systematic review of randomized trials for hepatocellular carcinoma treated with percutaneous ablation therapies. Hepatology. 2009;49:453–9.
Chinnaratha MA, Chuang MY, Fraser RJ, Woodman RJ, Wigg AJ. Percutaneous thermal ablation for primary hepatocellular carcinoma: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2016;31:294–301.
Kim YS, Lim HK, Rhim H, et al. Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol. 2013;58:89–97.
Bertot LC, Sato M, Tateishi R, Yoshida H, Koike K. Mortality and complication rates of percutaneous ablative techniques for the treatment of liver tumors: a systematic review. Eur Radiol. 2011;21:2584–96.
Solbiati L, Ahmed M, Cova L, Ierace T, Brioschi M, Goldberg SN. Small liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-up. Radiology. 2012;265:958–68.
Gillams AR, Lees WR. Five-year survival following radiofrequency ablation of small, solitary, hepatic colorectal metastases. J Vasc Interv Radiol. 2008;19:712–7.
Gillams AR, Lees WR. Five-year survival in 309 patients with colorectal liver metastases treated with radiofrequency ablation. Eur Radiol. 2009;19:1206–13.
Meloni MF, Andreano A, Laeseke PF, Livraghi T, Sironi S, Lee FT Jr. Breast cancer liver metastases: US-guided percutaneous radiofrequency ablation–intermediate and long-term survival rates. Radiology. 2009;253:861–9.
Oshowo A, Gillams AR, Lees WR, Taylor I. Radiofrequency ablation extends the scope of surgery in colorectal liver metastases. Eur J Surg Oncol. 2003;29:244–7.
Sofocleous CT, Petre EN, Gonen M, et al. CT-guided radiofrequency ablation as a salvage treatment of colorectal cancer hepatic metastases developing after hepatectomy. J Vasc Interv Radiol. 2011;22:755–61.
Bai H, Huangz X, Jing L, Zeng Q, Han L. The effect of radiofrequency ablation versus liver resection on survival outcome of colorectal liver metastases (CRLM): a meta-analysis. Hepatogastroenterology. 2015;62:373–7.
Weng M, Zhang Y, Zhou D, et al. Radiofrequency ablation versus resection for colorectal cancer liver metastases: a meta-analysis. PLoS ONE. 2012;7:e45493.
Liu Z, Ahmed M, Weinstein Y, Yi M, Mahajan RL, Goldberg SN. Characterization of the RF ablation-induced ‘oven effect’: the importance of background tissue thermal conductivity on tissue heating. Int J Hyperthermia. 2006;22:327–42.
Ahmed M, Liu Z, Afzal KS, et al. Radiofrequency ablation: effect of surrounding tissue composition on coagulation necrosis in a canine tumor model. Radiology. 2004;230:761–7.
Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999;210:655–61.
Terraz S, Constantin C, Majno PE, Spahr L, Mentha G, Becker CD. Image-guided multipolar radiofrequency ablation of liver tumours: initial clinical results. Eur Radiol. 2007;17:2253–61.
Goldberg SN, Grassi CJ, Cardella JF, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2009;20:S377–90.
Crocetti L, de Baere T, Lencioni R. Quality improvement guidelines for radiofrequency ablation of liver tumours. Cardiovasc Interv Radiol. 2010;33:11–7.
Salhab M, Canelo R. An overview of evidence-based management of hepatocellular carcinoma: a meta-analysis. J Cancer Res Ther. 2011;7:463–75.
Lencioni R, Crocetti L. Local-regional treatment of hepatocellular carcinoma. Radiology. 2012;262:43–58.
Wang Y, Luo Q, Li Y, Deng S, Wei S, Li X. Radiofrequency ablation versus hepatic resection for small hepatocellular carcinomas: a meta-analysis of randomized and nonrandomized controlled trials. PLoS ONE. 2014;9:e84484.
Qi X, Tang Y, An D, et al. Radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma: a meta-analysis of randomized controlled trials. J Clin Gastroenterol. 2014;48:450–7.
Peng ZW, Zhang YJ, Chen MS, Lin XJ, Liang HH, Shi M. Radiofrequency ablation as first-line treatment for small solitary hepatocellular carcinoma: long-term results. Eur J Surg Oncol. 2010;36:1054–60.
Zytoon AA, Ishii H, Murakami K, et al. Recurrence-free survival after radiofrequency ablation of hepatocellular carcinoma. A registry report of the impact of risk factors on outcome. Jpn J Clin Oncol. 2007;37:658–72.
Peng ZW, Zhang YJ, Chen MS, et al. Risk factors of survival after percutaneous radiofrequency ablation of hepatocellular carcinoma. Surg Oncol. 2008;17:23–31.
Mulier S, Ni Y, Frich L, et al. Experimental and clinical radiofrequency ablation: proposal for standardized description of coagulation size and geometry. Ann Surg Oncol. 2007;14:1381–96.
Shady W, Petre EN, Gonen M, et al. Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes–A 10-year experience at a single center. Radiology. 2016;278:601–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest regarding this study.
Informed Consent
The institutional review board approved this study and waived the informed consent requirement because of the retrospective nature of the study.
Rights and permissions
About this article
Cite this article
Cassinotto, C., Denys, A., Gay, F. et al. Radiofrequency Ablation of Liver Tumors: No Difference in the Ablation Zone Volume Between Cirrhotic and Healthy Liver. Cardiovasc Intervent Radiol 41, 905–911 (2018). https://doi.org/10.1007/s00270-018-1898-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-1898-z