Abstract
Background
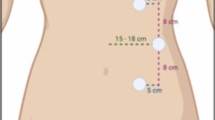
The anatomy of the transversus abdominis muscle and its aponeurosis is important in transversus abdominis release surgery. We studied the CT anatomy of the transversus abdominis muscle medial to the linea semilunaris at different levels in the abdomen and measured the thickness of this muscle.
Methods
In this retrospective study, we analysed 150 abdominal computed tomography at L1, L3, and L5 vertebral levels corresponding to subxiphoid, umbilical, and suprapubic regions, respectively. The patients were divided into three groups based on age and sex: women aged 15–20 years (nulliparous), women aged 30–60 years (multiparous), and men aged 15–60 years, with each group having 50 patients. We compared the thickness of the TA muscle at the L1 level between men and women and between nulliparous and multiparous women.
Results
Transversus abdominis muscle was consistently present medial to the linea semilunaris at L1 vertebral level in the subxiphoid region (150/150). At the L3 vertebral level in the mid-abdomen, only eight patients had the transversus abdominis muscle there (8/150, 5%). At the L5 vertebral level in the suprapubic region, no patient had the transversus abdominis muscle medial to the linea semilunaris. The mean thickness of the transversus abdominis muscle at the L1 level was 3.4 mm, and at the L3 level, it was 1.6 mm. There was no statistically significant difference in the transversus abdominis muscle thickness between the men and women; however, a significant difference was found between the nulliparous and multiparous women, with thinner TA muscle in later.
Conclusion
There is good transversus abdominis muscle bulk medial to the linea semilunaris for doing transversus abdominis muscle division in the upper abdomen. However, as we move towards the mid-abdomen, we have TA aponeurosis or rarely TA muscle of little bulk.



Similar content being viewed by others
References
Novitsky YW, Fayezizadeh M, Majumder A, Neupane R, Elliott HL, Orenstein SB (2016) Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg 264(2):226–232. https://doi.org/10.1097/SLA.0000000000001673
Pauli EM, Wang J, Petro CC, Juza RM, Novitsky YW, Rosen MJ (2015) Posterior component separation with transversus abdominis release successfully addresses recurrent ventral hernias following anterior component separation. Hernia 19:285–91
Petro CC, Como JJ, Yee S, Prabhu AS, Novitsky YW, Rosen MJ (2015) Posterior component separation and transversus abdominis muscle release for complex incisional hernia repair in patients with a history of an open abdomen. J Trauma Acute Care Surg 78:422–9
Sanford DE, Doyle MB, Chapman WC, Blatnik JA (2018) Transversus abdominus muscle release with mesh reinforcement is safe and effective for repairing incisional hernias in liver transplant patients. HPB 20:S808-9
Petro CC, Orenstein SB, Criss CN, Sanchez EQ, Rosen MJ, Woodside KJ et al (2015) Transversus abdominis muscle release for repair of complex incisional hernias in kidney transplant recipients. Am J Surg 210:334–9
Afaque MY, Rizvi AA (2020) Comparison between transversus abdominis release and anterior component separation technique in complex ventral hernia. Int J Abdom Wall Hernia Surg 3:81–6
Punekar I, Khouri JS, Catanzaro M, Shaikh AL, Langstein HN (2018) Redefining the rectus sheath: implications for abdominal wall repair. Plast Reconstr Surg 141(2):473–479. https://doi.org/10.1097/PRS.0000000000004043
Plumb AA, Windsor A, Ross D (2021) Contemporary imaging of rectus diastasis and the abdominal wall. Hernia J Hernias Abdom Wall Surg 25(4):921–927. https://doi.org/10.1007/s10029-021-02463-z
Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K (2016) Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Brit J Sports Med 50(17):1092–1096. https://doi.org/10.1136/bjsports-2016-096065
Cavalli M, Aiolfi A, Bruni PG, Manfredini L, Lombardo F, Bonfanti MT, Bona D, Campanelli G (2021) Prevalence and risk factors for diastasis recti abdominis: a review and proposal of a new anatomical variation. Hernia J Hernias Abdom Wall Surg 25(4):883–890. https://doi.org/10.1007/s10029-021-02468-8
Grossi JVM, Lee B, Belyansky I, Carbonell AM, Cavazzola LT, Novitsky YW, Ballecer CD (2021) Critical view of robotic-assisted transverse abdominal release (r-TAR). Hernia J Hernias Abdom Wall Surg 25(6):1715–1725. https://doi.org/10.1007/s10029-021-02391-y
Ramirez OM, Ruas E, Dellon AL (1990) Components separation’ method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86:519–26
Saulis AS, Dumanian GA (2002) Periumbilical rectus abdominis perforator preservation significantly reduces superficial wound complications in “separation of parts” hernia repairs. Plast Reconstr Surg 109:2275–80
Malik A, MacDonald ADH, De Beaux AC, Tulloh BR (2014) The peritoneal fap hernioplasty for repair of large ventral and incisional hernias. Hernia 18:39–45
Nielsen MF, de Beaux A, Tulloh B (2019) Peritoneal fap hernioplasty for reconstruction of large ventral hernias: long-term outcome in 251 patients. World J Surg 43:2157–2163. https://doi.org/10.1007/s00268-019-05011-0
Raynor RW, Del Guercio LR (1989) The place for pneumoperitoneum in the repair of massive hernia. World J Surg. 13(5):581–585. https://doi.org/10.1007/BF01658874
Motz BM, Schlosser KA, Heniford BT (2018) Chemical components separation: concepts, evidence, and outcomes. Plast Reconstr Surg. 142(3 Suppl):58S-63S. https://doi.org/10.1097/PRS.0000000000004856
Holihan JL, Karanjawala B, Ko A, Askenasy EP, Matta EJ, Gharbaoui L, Hasapes JP, Tammisetti VS, Thupili CR, Alawadi ZM, Bondre I, Flores-Gonzalez JR, Kao LS, Liang MK (2016) Use of computed tomography in diagnosing ventral hernia recurrence: a blinded, prospective. Multispec Eval JAMA Surg 151(1):7–13
Kroese LF, Sneiders D, Kleinrensink GJ, Muysoms F, Lange JF (2018) Comparing different modalities for the diagnosis of incisional hernia: a systematic review. Hernia 22(2):229–242
Kushner B, Starnes C, Sehnert M, Holden S, Blatnik J (2021) Identifying critical computed tomography (CT) imaging findings for the preoperative planning of ventral hernia repairs. Hernia J Hernias Abdom Wall Surg 25(4):963–969. https://doi.org/10.1007/s10029-020-02314-3
Afaque MY (2021) Assessing the complexity of ventral hernia by methods of Tanaka, Sabbagh, Carbonell, and Love. Hernia J Hernias Abdom Wall Surg 25(2):557–558. https://doi.org/10.1007/s10029-020-02267-7
Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK (2016) Mesh location in open ventral hernia repair: A systematic review and network meta-analysis. World J Surg 40(1):89–99. https://doi.org/10.1007/s00268-015-3252-9
Blair LJ, Cox TC, Huntington CR, Groene SA, Prasad T, Lincourt AE, Kercher KW, Heniford BT, Augenstein VA (2017) The effect of component separation technique on quality of life (QOL) and surgical outcomes in complex open ventral hernia repair (OVHR). Surg Endosc 31(9):3539–3546. https://doi.org/10.1007/s00464-016-5382-z
Lopez-Monclus J, Muñoz-Rodríguez J, San Miguel C et al (2020) Combining anterior and posterior component separation for extreme cases of abdominal wall reconstruction. Hernia 24(2):369–379. https://doi.org/10.1007/s10029-020-02152-3
Sneiders D, de Smet GHJ, den Hartog F et al (2021) Medialization after combined anterior and posterior component separation in giant incisional hernia surgery, an anatomical study. Surgery. 170(6):1749–1757. https://doi.org/10.1016/j.surg.2021.06.018
Baig SJ, Afaque MY, Priya P (2022) Combination of transversus abdominis release and peritoneal flap hernioplasty for large midline ventral hernias: a case series. Indian J Surg. https://doi.org/10.1007/s12262-021-03279-y
Baig SJ, Afaque MY (2022) TAR plus (TAR plus peritoneal flap hernioplasty) for large midline ventral hernias. In: Baig SJ, Bhandarkar D, Priya P (eds) Newer concepts and procedures in hernia surgery—an Atlas. Springer, Singapore. https://doi.org/10.1007/978-981-19-5248-7_19
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare there is no conflict of interest.
Ethics approval
Institutional ethical approval (including appropriate approvals or waivers) was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Afaque, M.Y., Qaseem, S.M.D., Shah, M.A. et al. Surgical Anatomy of Transversus Abdominis Muscle for Transversus Abdominis Release: A CT-Based Study in Three Patient Groups. World J Surg 47, 2718–2723 (2023). https://doi.org/10.1007/s00268-023-07163-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07163-6