Abstract
Background
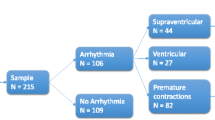
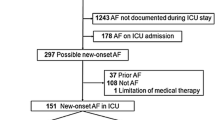
Arrhythmias are common in critically ill patients, though the impact of arrhythmias on surgical patients is not well delineated. We aimed to characterize mortality following arrhythmias in critically ill patients.
Methods
We performed a propensity-matched retrospective analysis of intensive care unit (ICU) patients from 2007 to 2017 in the Cerner Acute Physiology and Chronic Health Evaluation database. We compared outcomes between patients with and without arrhythmias and those with and without surgical indications for ICU admission. We also modeled predictors of arrhythmias in surgical patients.
Results
467,951 patients were included; 97,958 (20.9%) were surgical patients. Arrhythmias occurred in 1.4% of the study cohorts. Predictors of arrhythmias in surgical patients included a history of cardiovascular disease (odds ratio [OR] 1.35, 95% confidence interval [CI95] 1.11–1.63), respiratory failure (OR 1.48, CI95 1.12–1.96), pneumonia (OR 3.17, CI95 1.98–5.10), higher bicarbonate level (OR 1.03, CI95 1.01–1.05), lower albumin level (OR 0.79, CI95 0.68–0.91), and vasopressor requirement (OR 27.2, CI95 22.0–33.7). After propensity matching, surgical patients with arrhythmias had a 42% mortality risk reduction compared to non-surgical patients (risk ratio [RR] 0.58, CI 95 0.43–0.79). Predicted probabilities of mortality for surgical patients were lower at all ages.
Conclusions
Surgical patients with arrhythmias are at lower risk of mortality than non-surgical patients. In this propensity-matched analysis, predictors of arrhythmias in critically ill surgical patients included a history of cardiovascular disease, respiratory complications, increased bicarbonate levels, decreased albumin levels, and vasopressor requirement. These findings highlight the differential effect of arrhythmias on different cohorts of critically ill populations.

Similar content being viewed by others
References
Reinelt P, Karth GD, Geppert A et al (2001) Incidence and type of cardiac arrhythmias in critically ill patients: a single center experience in a medical-cardiological ICU. Intensive Care Med 27(9):1466–1473
Annane D, Sebille V, Duboc D et al (2008) Incidence and prognosis of sustained arrhythmias in critically ill patients. Am J Respir Crit Care Med 178(1):20–25
Wong DT, Cheng D, Kustra R et al (1999) Risk factors of delayed extubation, prolonged length of stay in the intensive care unit, and mortality in patients undergoing coronary artery bypass graft with fast-track cardiac anesthesia. Anesthesiology 91:936–944
Tse G (2016) Mechanisms of cardiac arrhythmias. J Arrhythm 32(2):75–81
Antzelevitch C, Burashnikov A (2011) Overview of basic mechanisms of cardiac arrhythmia. Card Electrophysiol Clin 3(1):23–45
Coumel P (1989) Classification of human arrhythmias. In: Vaughan Williams EM (ed) Antiarrhythmic drugs. Handbook of experimental pharmacology, vol 89. Springer, Berlin Heidelberg
Chung MK, Martin DO, Sprecher D et al (2001) C-reactive protein elevation in patients with atrial arrhythmias: inflammatory mechanisms and persistence of atrial fibrillation. Circulation 104:2886–3289
Kanji S, Williamson DR, Yaghchi BM, et al. Canadian Critical Care Trials Group (2012) Epidemiology and management of atrial fibrillation in medical and noncardiac surgical adult intensive care unit patients. J Crit Care, 27(3):326.e1–326.e3268
Echahidi N, Pibarot P, O’Hara G et al (2008) Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol 51(8):793–801
Gillinov AM, Bagiella E, Moskowitz AJ et al (2016) Rate control versus rhythm control for atrial fibrillation after cardiac surgery. N Engl J Med 374(20):1911–1921
Ganguly S, Brown T, Pritchett C et al (2015) Atrial fibrillation in intensive care. Intensive Care Med Exp 3(Suppl 1):A209
Guenancia C, Binquet C, Laurent G et al (2015) Incidence and predictors of new-onset atrial fibrillation in septic shock patients in a medical ICU: data from 7-day holter ECG monitoring. PLoS ONE 10(5):e0127168
Zimmerman JE, Kramer AA, McNair DS et al (2006) Acute physiology and chronic health evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med 34(5):1297–1310
Knaus WA, Wagner DP, Draper EA et al (1991) The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100(6):1619–1636
Dobrev D, Aguilar M, Heijman J et al (2019) Postoperative atrial fibrillation: mechanisms, manifestations and management. Nat Rev Cardiol 16(7):417–436
Wetterslev M, Hylander Møller M, Granholm A et al (2023) Atrial fibrillation (AFIB) in the ICU: incidence, risk factors, and outcomes: the international AFIB-ICU cohort study. Crit Care Med. https://doi.org/10.1097/CCM.0000000000005883
Arrigo M, Ishihara S, Feliot E et al (2018) New-onset atrial fibrillation in critically ill patients and its association with mortality: a report from the FROG-ICU study. Int J Cardiol 266:95–99
Meierhenrich R, Steinhilber E, Eggermann C et al (2010) Incidence and prognostic impact of new-onset atrial fibrillation in patients with septic shock: a prospective observational study. Crit Care 14(3):R108
Healey JS, Connolly SJ, Gold MR, et al. (2012) Subclinical atrial fibrillation and the risk of stroke [published correction appears in N Engl J Med. 2016 Mar 10;374(10):998]. N Engl J Med, 366(2):120–129.
Valderrábano RJ, Blanco A, Santiago-Rodriguez EJ et al (2016) Risk factors and clinical outcomes of arrhythmias in the medical intensive care unit. J Intensive Care 4:9
Bosch NA, Cimini J, Walkey AJ (2018) Atrial fibrillation in the ICU. Chest 154(6):1424–1434
Christian SA, Schorr C, Ferchau L et al (2008) Clinical characteristics and outcomes of septic patients with new-onset atrial fibrillation. J Crit Care 23(4):532–536
Walkey AJ, Wiener RS, Ghobrial JM et al (2011) Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA 306(20):2248–2254
Bruins P, te Velthuis H, Yazdanbakhsh AP et al (1997) Activation of the complement system during and after cardiopulmonary bypass surgery: postsurgery activation involves C-reactive protein and is associated with postoperative arrhythmia. Circulation 96(10):3542–3548
van Beek DEC, Kuijpers YAM, Königs MHH et al (2020) Low serum albumin levels and new-onset atrial fibrillation in the ICU: a prospective cohort study. J Crit Care 56:26–30
Saliba W, Wazni OM (2011) Sinus rhythm restoration and treatment success: insight from recent clinical trials. Clin Cardiol 34(1):12–22
Shahreyar M, Fahhoum R, Akinseye O et al (2018) Severe sepsis and cardiac arrhythmias. Ann Transl Med 6(1):6
POISE Study Group, Devereaux PJ, Yang H et al (2008) Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet 371(9627):1839–1847
Bangalore S, Wetterslev J, Pranesh S et al (2008) Perioperative beta blockers in patients having non-cardiac surgery: a meta-analysis. Lancet 372(9654):1962–1976
Walkey AJ, Myers LC, Thai KK et al (2023) Practice patterns and outcomes associated with anticoagulation use following sepsis hospitalizations with new-onset atrial fibrillation. Circ Cardiovasc Qual Outcomes 16(3):e009494
Rahman F, Wang N, Yin X et al (2016) Atrial flutter: clinical risk factors and adverse outcomes in the Framingham Heart Study. Heart Rhythm 13(1):233–240
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
This study was approved by the Institutional Review Boards at the University of North Carolina and the University of Minnesota.
Informed consent
Informed consent was waived for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
An, S.J., Davis, D., Peiffer, S. et al. Arrhythmias in Critically Ill Surgical and Non-surgical Patients: A National Propensity-Matched Study. World J Surg 47, 2668–2675 (2023). https://doi.org/10.1007/s00268-023-07129-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07129-8