Abstract
Background
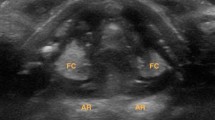
Vocal cord paresis (VCP) is a serious complication after esophagectomy. Conventional diagnosis of VCP relies on flexible laryngoscopy (FL), which is invasive. Laryngeal ultrasonography (LUSG) is non-invasive and convenient. It has provided accurate VC evaluation after thyroidectomy but it is unclear if it is just as accurate following esophagectomy. This prospective study evaluated the feasibility and accuracy of LUSG in VC assessment on day-1 after esophagectomy.
Methods
Consecutive patients from a tertiary teaching hospital who underwent elective esophagectomy were prospectively recruited. All received pre-operative FL, and post-operative LUSG and FL on Day-1, each performed by a blinded, independent assessor. The primary outcomes were feasibility and accuracy of LUSG in the diagnosis of VCP on Day-1 post-esophagectomy. The accuracy of voice assessment (VA) was analyzed.
Results
Twenty-six patients were eligible for analysis. The median age was 70 years (66–73). Majority were male (84.6%). Twenty-five (96.2%) received three-phase esophagectomy. Twenty-four (96%) had same-stage anastomosis at the neck. Three (11.5%) developed temporary and one (3.8%) developed permanent unilateral VCP. Overall VC visualization rate by LUSG was 100%; sensitivity, specificity, positive predictive value, negative predictive value (NPV) and accuracy of LUSG were 75.0%, 100%, 100%, 98.0%, 98.1% respectively, and superior to VA. Combining LUSG with VA findings could pick up all VCPs i.e. improved sensitivity and NPV to 100%.
Conclusion
LUSG is a highly feasible, accurate and non-invasive method to evaluate VC function early after esophagectomy. Post-operative FL may be avoided in patients with both normal LUSG and voice.



Similar content being viewed by others
References
Scholtemeijer MG, Seesing MFJ, Brenkman HJF et al (2017) Recurrent laryngeal nerve injury after esophagectomy for esophageal cancer: incidence, management, and impact on short- and long-term outcomes. J Thorac Dis 9:S868–S878. https://doi.org/10.21037/jtd.2017.06.92
Sato Y, Kosugi S, Aizawa N et al (2016) Risk factors and clinical outcomes of recurrent laryngeal nerve paralysis after esophagectomy for thoracic esophageal carcinoma. World J Surg 40:129–136. https://doi.org/10.1007/s00268-015-3261-8
Oshikiri T, Takiguchi G, Hasegawa H et al (2021) Postoperative recurrent laryngeal nerve palsy is associated with pneumonia in minimally invasive esophagectomy for esophageal cancer. Surg Endosc 35:837–844. https://doi.org/10.1007/s00464-020-07455-1
Friedman AD, Burns JA, Heaton JT, Zeitels SM (2010) Early versus late injection medialization for unilateral vocal cord paralysis. Laryngoscope 120:2042–2046. https://doi.org/10.1002/lary.21097
Yung KC, Likhterov I, Courey MS (2011) Effect of temporary vocal fold injection medialization on the rate of permanent medialization laryngoplasty in unilateral vocal fold paralysis patients. Laryngoscope 121:2191–2194. https://doi.org/10.1002/lary.21965
Paul BC, Rafii B, Achlatis S et al (2012) Morbidity and patient perception of flexible laryngoscopy. Ann Otol Rhinol Laryngol 121(11):708–713
Lammers MJW, Lea J, Lea J, Westerberg BD (2020) Guidance for otolaryngology health care workers performing aerosol generating medical procedures during the COVID-19 pandemic. J Otolaryngol Head Neck Surg 49:1–8. https://doi.org/10.1186/s40463-020-00429-2
Fung MMH, Lang BHH (2021) A prospective study evaluating the feasibility and accuracy of very early postoperative translaryngeal ultrasonography in the assessment of vocal cord function after neck surgery. Surgery (United States) 169:191–196. https://doi.org/10.1016/j.surg.2020.03.025
Dedecjus M, Adamczewski Z, Brzeziński J, Lewiński A (2010) Real-time, high-resolution ultrasonography of the vocal folds-a prospective pilot study in patients before and after thyroidectomy. Langenbecks Arch Surg 395:859–864. https://doi.org/10.1007/s00423-010-0694-2
Wong KP, Lang BHH, Ng SH et al (2013) A prospective, assessor-blind evaluation of surgeon-performed transcutaneous laryngeal ultrasonography in vocal cord examination before and after thyroidectomy. Surgery (United States) 154:1158–1165. https://doi.org/10.1016/j.surg.2013.04.063
Carneiro-Pla D, Miller BS, Wilhelm SM et al (2014) Feasibility of surgeon-performed transcutaneous vocal cord ultrasonography in identifying vocal cord mobility: a multi-institutional experience. Surgery (United States) 156:1597–1604. https://doi.org/10.1016/j.surg.2014.08.071
Woo JW, Park I, Choe JH, et al (2017) Comparison of ultrasound frequency in laryngeal ultrasound for vocal cord evaluation. In: Surgery (United States). Mosby Inc., pp 1108–1112
De Miguel M, Peláez EM, Caubet E et al (2017) Accuracy of transcutaneous laryngeal ultrasound for detecting vocal cord paralysis in the immediate postoperative period after total thyroidectomy. Minerva Anestesiol 83:1239–1247. https://doi.org/10.23736/S0375-9393.17.11755-4
Lazard DS, Bergeret-Cassagne H, Lefort M et al (2018) Transcutaneous laryngeal ultrasonography for laryngeal immobility diagnosis in patients with voice disorders after thyroid/parathyroid surgery. World J Surg 42:2102–2108. https://doi.org/10.1007/s00268-017-4428-2
Knyazeva P, Makarin V, Seeliger B et al (2018) Transcutaneous laryngeal ultrasonography (TLUS) as an alternative to direct flexible laryngoscopy (DFL) in the perioperative evaluation of the vocal cord mobility in thyroid surgery. Langenbecks Arch Surg 403:1015–1020. https://doi.org/10.1007/s00423-018-1734-6
Shah MK, Ghai B, Bhatia N et al (2019) Comparison of transcutaneous laryngeal ultrasound with video laryngoscope for assessing the vocal cord mobility in patients undergoing thyroid surgery. Auris Nasus Larynx 46:593–598. https://doi.org/10.1016/j.anl.2018.12.007
Fung MMH, Lang BH-H (2021) A prospective study comparing the midline and lateral trans-laryngeal ultrasonography approaches in vocal cord assessment before and after thyroid and neck surgeries. Am J Surg. https://doi.org/10.1016/j.amjsurg.2021.06.016
Fujihata S, Ogawa R, Ito S et al (2021) Diagnosis of recurrent laryngeal nerve paralysis following esophagectomy by evaluating movement of the vocal cords and arytenoid cartilages using ultrasonography. Esophagus 18:704–709. https://doi.org/10.1007/s10388-021-00830-4
Leng X, Teng X, Xu S et al (2022) 360. Diagnosis of recurrent laryngeal nerve paralysis by evaluating movement of the vocal cords using ultrasonography after minimally invasive esophagectomy. Dis Esophagus 35:doac051.360. https://doi.org/10.1093/dote/doac051.360
Chandrasekhar SS, Randolph GW, Seidman MD et al (2013) Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol—Head Neck Surg (USA). https://doi.org/10.1177/0194599813487301
Wong KP, Lang BHH, Lam S, et al (2016) Determining the learning curve of transcutaneous laryngeal ultrasound in vocal cord assessment by CUSUM analysis of eight surgical residents: when to abandon laryngoscopy. In: world journal of surgery. Springer, New York LLC, pp 659–664
Funding
The authors received no funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors had nothing to disclose. The authors had no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fung, M.MH., Wong, I.Yh., Chan, F.SY. et al. A Prospective Study Evaluating the Feasibility and Accuracy of Post-operative Laryngeal Ultrasonography (LUSG) in Assessment of Vocal Cord Function After Esophagectomy. World J Surg 47, 2792–2799 (2023). https://doi.org/10.1007/s00268-023-07128-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07128-9