Abstract
Background
Surgery is often a complex process that requires detailed 3-dimensional anatomical knowledge and rigorous interplay between team members to attain ideal operational efficiency or “flow.” Virtual Reality (VR) represents a technology by which to rehearse complex plans and communicate precise steps to a surgical team prior to entering the operating room. The objective of this study was to evaluate the use of VR for preoperative surgical team planning and interdisciplinary communication across all surgical specialties.
Methods
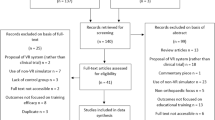
A systematic review of the literature was performed examining existing research on VR use for preoperative surgical team planning and interdisciplinary communication across all surgical fields in order to optimize surgical efficiency. MEDLINE, SCOPUS, CINAHL databases were searched from inception to July 31, 2022 using standardized search clauses. A qualitative data synthesis was performed with particular attention to preoperative planning, surgical efficiency optimization, and interdisciplinary collaboration/communication techniques determined a priori. Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines were followed. All included studies were appraised for their quality using the Medical Education Research Study Quality Instrument (MERSQI) tool.
Results
One thousand and ninety-three non-duplicated articles with abstract and full text availability were identified. Thirteen articles that examined preoperative VR-based planning techniques for optimization of surgical efficiency and/or interdisciplinary communication fulfilled inclusion and exclusion criteria. These studies had a low-to-medium methodological quality with a MERSQI mean score of 10.04 out of 18 (standard deviation 3.61).
Conclusions
This review demonstrates that time spent rehearsing and visualizing patient-specific anatomical relationships in VR may improve operative efficiency and communication across multiple surgical specialties.

Similar content being viewed by others
References
Köckerling F, Sheen AJ, Berrevoet F, Campanelli G, Cuccurullo D, Fortelny R et al (2019) The reality of general surgery training and increased complexity of abdominal wall hernia surgery. Hernia 23(6):1081–1091
Moridzadeh RS, Sanaiha Y, Madrigal J, Antonios J, Benharash P, Baril DT (2021) Nationwide comparison of the medical complexity of patients by surgical specialty. J Vasc Surg 73(2):683–688
Horner W, Peng K, Pleasant V, Brackmann M, Ebott J, Gutfreund R et al (2019) Trends in surgical complexity and treatment modalities utilized in the management of ovarian cancer in an era of neoadjuvant chemotherapy. Gynecol Oncol 154(2):283–289
De Salvatore S, Vadalà G, Oggiano L, Russo F, Ambrosio L, Costici PF (2021) Virtual reality in preoperative planning of adolescent idiopathic scoliosis surgery using google cardboard. Neurospine 18(1):199–205
Parkhomenko E, O’Leary M, Safiullah S, Walia S, Owyong M, Lin C et al (2019) Pilot assessment of immersive virtual reality renal models as an educational and preoperative planning tool for percutaneous nephrolithotomy. J Endourol 33(4):283–288
Chen S, Zhang K, Jia X, Qiang M, Chen Y (2020) Evaluation of the computer-assisted virtual surgical technology in preoperative planning for distal femoral fracture. Injury 51(2):443–451
Tack P, Victor J, Gemmel P, Annemans L (2016) 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online 15(1):115
Tan LA, Yerneni K, Tuchman A, Li XJ, Cerpa M, Lehman RA et al (2018) Utilization of the 3D-printed spine model for freehand pedicle screw placement in complex spinal deformity correction. J Spine Surg 4(2):319–327
Lopez CD, Boddapati V, Lee NJ, Dyrszka MD, Sardar ZM, Lehman RA et al (2021) Three-dimensional printing for preoperative planning and pedicle screw placement in adult spinal deformity: a systematic review. Global Spine J 11(6):936–949
Wagner JD, Baack B, Brown GA, Kelly J (2004) Rapid 3-dimensional prototyping for surgical repair of maxillofacial fractures: a technical note. J Oral Maxillofac Surg 62(7):898–901
Bagaria V, Deshpande S, Rasalkar DD, Kuthe A, Paunipagar BK (2011) Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. Eur J Radiol 80(3):814–820
Ballard DH, Mills P, Duszak R, Weisman JA, Rybicki FJ, Woodard PK (2020) Medical 3D printing cost-savings in orthopedic and maxillofacial surgery: cost analysis of operating room time saved with 3D printed anatomic models and surgical guides. Acad Radiol 27(8):1103–1113
Lupulescu C, Sun Z (2019) A systematic review of the clinical value and applications of three-dimensional printing in renal surgery. J Clin Med 8(7):E990
Treadwell JR, Lucas S, Tsou AY (2014) Surgical checklists: a systematic review of impacts and implementation. BMJ Qual Saf 23(4):299–318
Marr M, Hemmert K, Nguyen AH, Combs R, Annamalai A, Miller G et al (2012) Team play in surgical education: a simulation-based study. J Surg Educ 69(1):63–69
Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AHS, Dellinger EP et al (2009) A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 360(5):491–499
Daniels K, Auguste T (2013) Moving forward in patient safety: multidisciplinary team training. Semin Perinatol 37(3):146–150
Butterworth K, Anderson K, Hedgeland T, Colyar T (2021) Encouraging interdisciplinary preoperative communication with a virtual huddle. AORN J 114(2):173–180
Lungu AJ, Swinkels W, Claesen L, Tu P, Egger J, Chen X (2021) A review on the applications of virtual reality, augmented reality and mixed reality in surgical simulation: an extension to different kinds of surgery. Expert Rev Med Devices 18(1):47–62
Yan C, Wu T, Huang K, He J, Liu H, Hong Y et al (2021) The application of virtual reality in cervical spinal surgery: a review. World Neurosurg 145:108–113
Godzik J, Farber SH, Urakov T, Steinberger J, Knipscher LJ, Ehredt RB et al (2021) “Disruptive technology” in spine surgery and education: virtual and augmented reality. Oper Neurosurg (Hagerstown) 21(Suppl 1):S85–S93
Ghaednia H, Fourman MS, Lans A, Detels K, Dijkstra H, Lloyd S et al (2021) Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J 21(10):1617–1625
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):n71
Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM (2007) Association between funding and quality of published medical education research. JAMA 298(9):1002–1009
Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH et al (2012) Development of a new knee society scoring system. Clin Orthop Relat Res 470(1):20–32
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–83
Hayes MHS, Patterson DG (1921) Experimental development of the graphic rating method. Psychol Bull 18:98–99
Chheang V, Fischer V, Buggenhagen H, Huber T, Huettl F, Kneist W et al (2020) Toward interprofessional team training for surgeons and anesthesiologists using virtual reality. Int J Comput Assist Radiol Surg 15(12):2109–2118
Kenngott HG, Pfeiffer M, Preukschas AA, Bettscheider L, Wise PA, Wagner M et al (2022) IMHOTEP: cross-professional evaluation of a three-dimensional virtual reality system for interactive surgical operation planning, tumor board discussion and immersive training for complex liver surgery in a head-mounted display. Surg Endosc 36(1):126–134
Likert R (1932) A technique for the measurement of attitudes [Ph. D.]. Columbia University
Kockro RA, Killeen T, Ayyad A, Glaser M, Stadie A, Reisch R et al (2016) Aneurysm surgery with preoperative three-dimensional planning in a virtual reality environment: technique and outcome analysis. World Neurosurg 96:489–499
Banks JL, Marotta CA (2007) Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials. Stroke 38(3):1091–1096
Louis RG, Steinberg GK, Duma C, Britz G, Mehta V, Pace J et al (2021) Early experience with virtual and synchronized augmented reality platform for preoperative planning and intraoperative navigation: a case series. Oper Neurosurg (Hagerstown) 21(4):189–196
McDonald M, Shirk DJ (2021) Application of three-dimensional virtual reality models to improve the pre-surgical plan for robotic partial nephrectomy. JSLS 25(3):e2021.00011
Shakya S, Li KD, Huang D, Liu ZQ, Zhang X, Liu L (2022) Virtual surgical planning is a useful tool in the surgical management of mandibular condylar fractures. Chin J Traumatol 25(3):151–155
Shirk JD, Thiel DD, Wallen EM, Linehan JM, White WM, Badani KK et al (2019) Effect of 3-dimensional virtual reality models for surgical planning of robotic-assisted partial nephrectomy on surgical outcomes: a randomized clinical trial. JAMA Netw Open 2(9):e1911598
Steineke TC, Barbery D (2021) Microsurgical clipping of middle cerebral artery aneurysms: preoperative planning using virtual reality to reduce procedure time. Neurosurg Focus 51(2):E12
Sugiyama T, Clapp T, Nelson J, Eitel C, Motegi H, Nakayama N et al (2021) Immersive 3-dimensional virtual reality modeling for case-specific presurgical discussions in cerebrovascular neurosurgery. Oper Neurosurg (Hagerstown) 20(3):289–299
Zheng C, Li J, Zeng G, Ye W, Sun J, Hong J et al (2019) Development of a virtual reality preoperative planning system for postlateral endoscopic lumbar discectomy surgery and its clinical application. World Neurosurg 123:e1–e8
Pfandler M, Lazarovici M, Stefan P, Wucherer P, Weigl M (2017) Virtual reality-based simulators for spine surgery: a systematic review. Spine J 17(9):1352–1363
Kirkman MA, Ahmed M, Albert AF, Wilson MH, Nandi D, Sevdalis N (2014) The use of simulation in neurosurgical education and training. A systematic review. J Neurosurg 121(2):228–246
Funding
The authors of this study do not have any financial support to disclose. No funding was necessary or received for the completion of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study do not have any conflicts of interests or financial conflicts to disclose.
Previous Presentations
This study has not been presented in part or in whole at a scientific meeting.
Previous Publications
This study has not been published in part or in whole in another journal.
Informed Consent
Internal Review Board Approval nor informed consent was not necessary for the completion of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Laskay, N.M.B., George, J.A., Knowlin, L. et al. Optimizing Surgical Performance Using Preoperative Virtual Reality Planning: A Systematic Review. World J Surg 47, 2367–2377 (2023). https://doi.org/10.1007/s00268-023-07064-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07064-8