Abstract
Background
Hospital length of stay (LOS) has been used as a surgical quality metric. This study seeks to determine the safety and feasibility of right colectomy as a ≤24-h short-stay procedure for colon cancer patients.
Methods
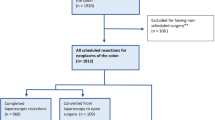
This was a retrospective cohort study using the ACS-NSQIP database and its Procedure Targeted Colectomy database (2012–2020). Adult patients with colon cancer who underwent right colectomies were identified. Patients were categorized into LOS ≤1 day (≤24-h short-stay), LOS 2–4 days, LOS 5–6 days, and LOS ≥7 days groups. Primary outcomes were 30-day overall and serious morbidity. Secondary outcomes were 30-day mortality, readmission, and anastomotic leak. The association between LOS and overall and serious morbidity was assessed using multivariable logistic regression.
Results
19,401 adult patients were identified, with 371 patients (1.9%) undergoing short-stay right colectomies. Patients undergoing short-stay surgery were generally younger with fewer comorbidities. Overall morbidity for the short-stay group was 6.5%, compared to 11.3%, 23.4%, and 42.0% for LOS 2–4 days, LOS 5–6 days, and LOS ≥7 days groups, respectively (p < 0.001). There were no differences in anastomotic leak, mortality, and readmission rates in the short-stay group compared to patients with LOS 2–4 days. Patients with LOS 2–4 days had increased odds of overall morbidity (OR 1.71, 95% CI 1.10–2.65, p = 0.016) compared to patients with short-stay but no differences in odds of serious morbidity (OR 1.20, 95% CI 0.61–2.36, p = 0.590).
Conclusions
≤24-h short-stay right colectomy is safe and feasible for a highly-select group of colon cancer patients. Optimizing patients preoperatively and implementing targeted readmission prevention strategies may aid patient selection.

Similar content being viewed by others
References
Hauck K, Zhao X (2011) How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med Care 49(12):1068–1075
Kelly KN, Iannuzzi JC, Aquina CT et al (2015) Timing of discharge: a key to understanding the reason for readmission after colorectal surgery. J Gastrointest Surg 19(3):418–427
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152(3):292–298
Brindle M, Nelson G, Lobo DN et al (2020) Recommendations from the ERAS® Society for standards for the development of enhanced recovery after surgery guidelines. BJS Open 4(1):157–163
Lovely JK, Maxson PM, Jacob AK et al (2012) Case-matched series of enhanced versus standard recovery pathway in minimally invasive colorectal surgery. Br J Surg 99(1):120–126
Korsholm M, Mogensen O, Jeppesen MM et al (2017) Systematic review of same-day discharge after minimally invasive hysterectomy. Int J Gynaecol Obstet 136(2):128–137
Gurusamy K, Junnarkar S, Farouk M et al (2008) Meta-analysis of randomized controlled trials on the safety and effectiveness of day-case laparoscopic cholecystectomy. Br J Surg 95(2):161–168
Abaza R, Martinez O, Ferroni MC et al (2019) Same day discharge after robotic radical prostatectomy. J Urol 202(5):959–963
Studniarek A, Borsuk DJ, Kochar K (2021) Feasibility assessment of outpatient colorectal resections at a tertiary referral center. Int J Colorectal Dis 36(3):501–508
Gignoux B, Gosgnach M, Lanz T et al (2019) Short-term outcomes of ambulatory colectomy for 157 consecutive patients. Ann Surg 270(2):317–321
McKenna NP, Bews KA, Shariq OA et al (2020) Is same-day and next-day discharge after laparoscopic colectomy reasonable in select patients? Dis Colon Rectum 63(10):1427–1435
Saadat LV, Mahvi DA, Jolissaint JS et al (2020) Twenty-three-hour-stay colectomy without increased readmissions: an analysis of 1905 cases from the national surgical quality improvement program. World J Surg 44(3):947–956
American College of Surgeons. About ACS-NSQIP. Accessed March 1, 2022. https://www.facs.org/quality-programs/acs-nsqip/about
American College of Surgeons. ACS NSQIP Participant Use Data File. Accessed March 1, 2022. https://www.facs.org/quality-programs/acs-nsqip/participant-use
Dindo D, Demartines N, Clavian PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Hosmer DWLS, Sturdivant RX (2000) Applied logistic regession, 2nd edn. Wiley, New York
Cologne KG, Byers S, Rosen DR et al (2016) Factors associated with a short (<2 days) or long (>10 days) length of stay after colectomy: a multivariate analysis of over 400 patients. Am Surg 82(10):960–963
Lian L, Kalady M, Geisler D et al (2010) Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc 24(8):2039–2043
Levy BF, Scott MJP, Fawcett WJ et al (2009) 23-hour-stay laparoscopic colectomy. Dis Colon Rectum 52(7):1239–1243
Wick EC, Shore AD, Hirose K et al (2011) Readmission rates and cost following colorectal surgery. Dis Colon Rectum 54(12):1475–1479
Asgeirsson T, El-Badawi K, Mahmood A et al (2010) Postoperative ileus: it costs more than you expect. J Am Coll Surg 210(2):228–231
Iyer S, Saunders WB, Stemkowski S (2009) Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm 15(6):485–494
Hyde LZ, Kiely JM, Al-Mazrou A et al (2019) Alvimopan significantly reduces length of stay and costs following colorectal resection and ostomy reversal even within an enhanced recovery protocol. Dis Colon Rectum 62(6):755–761
Henning RE, Hu KY, Rein LE et al (2019) Alvimopan is associated with decreased length of stay for both open and laparoscopic segmental colectomy. Surgery 166(4):483–488
Acknowledgements
Sophia Y. Chen and Shannon R. Radomski received financial support from National Cancer Institute (NCI) Grant 5T32CA126607-12. Mr. Edwin Lewis provided generous support of Dr. Efron's Department of Surgery Research Fund. The Nicholl Family Foundation provided generous support of the Johns Hopkins Division of Colorectal Surgery Research Fund. The authors would like to acknowledge the Johns Hopkins Surgery Center for Outcomes (JSCOR) for supporting this study.
Funding
Sophia Y. Chen and Shannon R. Radomski received financial support from National Cancer Institute (NCI) Grant 5T32CA126607-12. Mr. Edwin Lewis provided generous support of Dr. Efron's Department of Surgery Research Fund. The Nicholl Family Foundation provided generous support of the Johns Hopkins Division of Colorectal Surgery Research Fund.
Author information
Authors and Affiliations
Contributions
Study design: SYC, SNR, MS, BDL, JEE, BS, CA. Data acquisition and analysis: SYC, SNR, MS, BDL. Interpretation of data: SYC, SNR, MS, BDL, JEE, BS, CA. Drafting work: SYC, SNR, MS, BDL. Critical revision: SYC, SNR, MS, BDL, JEE, BS, CA. Final approval/accountability: SYC, SNR, MS, BDL, JEE, BS, CA.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, S.Y., Radomski, S.N., Stem, M. et al. Safety and Feasibility of ≤24-h Short-Stay Right Colectomies for Primary Colon Cancer. World J Surg 47, 2267–2278 (2023). https://doi.org/10.1007/s00268-023-07041-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07041-1