Abstract
Background
Gastroschisis mortality in sub-Saharan Africa (SSA) remains high at 59–100%. Silo inaccessibility contributes to this disparity. Standard of care (SOC) silos cost $240, while median monthly incomes in SSA are < $200. Our multidisciplinary American and Ugandan team designed and bench-tested a low-cost (LC) silo that costs < $2 and is constructed from locally available materials. Here we describe in vivo LC silo testing.
Methods
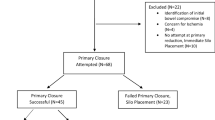
A piglet gastroschisis model was achieved by eviscerating intestines through a midline incision. Eight piglets were randomized to LC or SOC silos. Bowel was placed into the LC or SOC silo, maintained for 1-h, and reduced. Procedure times for placement, intestinal reduction, and silo removal were recorded. Tissue injury of the abdominal wall and intestine was assessed. Bacterial and fungal growth on silos was also compared.
Results
There were no gross injuries to abdominal wall or intestine in either group or difference in minor bleeding. Times for silo application, bowel reduction, and silo removal between groups were not statistically or clinically different, indicating similar ease of use. Microbiologic analysis revealed growth on all samples, but density was below the standard peritoneal inoculum of 105 CFU/g for both silos. There was no significant difference in bacterial or fungal growth between LC and SOC silos.
Conclusion
LC silos designed for manufacturing and clinical use in SSA demonstrated similar ease of use, absence of tissue injury, and acceptable microbiology profile, similar to SOC silos. The findings will allow our team to proceed with a pilot study in Uganda.





Similar content being viewed by others
Abbreviations
- LC:
-
Low cost
- SOC:
-
Standard of care
- LMICs:
-
Low- and middle-income countries
- SSA:
-
Sub-Saharan Africa
References
Ullrich SJ, Kakembo N, Grabski DF et al (2020) Burden and outcomes of neonatal surgery in Uganda: results of a five-year prospective study. J Surg Res 246:93–99. https://doi.org/10.1016/j.jss.2019.08.015
Gamba P, Midrio P (2014) Abdominal wall defects: prenatal diagnosis, newborn management, and long-term outcomes. Semin Pediatr Surg 23(5):283–290. https://doi.org/10.1053/j.sempedsurg.2014.09.009
Ford K, Poenaru D, Moulot O et al (2016) Gastroschisis: Bellwether for neonatal surgery capacity in low resource settings? J Pediatr Surg 51(8):1262–1267. https://doi.org/10.1016/j.jpedsurg.2016.02.090
Wesonga AS, Fitzgerald TN, Kabuye R et al (2016) Gastroschisis in Uganda: opportunities for improved survival. J Pediatr Surg 51(11):1772–1777. https://doi.org/10.1016/j.jpedsurg.2016.07.011
Wesonga A, Situma M, Lakhoo K (2020) Reducing gastroschisis mortality: a quality improvement initiative at a Ugandan pediatric surgery unit. World J Surg 44(5):1395–1399. https://doi.org/10.1007/s00268-020-05373-w
Arivoli M, Biswas A, Burroughs N et al (2020) Multidisciplinary development of a low-cost gastroschisis silo for use in Sub-Saharan Africa. J Surg Res 255:565–574. https://doi.org/10.1016/j.jss.2020.05.037
Swift RISM, Ziderman DA, Silverman M, Elder MA, Elder MG (1992) A new regime in the management of gastroschisis. J Pediatr Surg 27(1):61–63
Novotny DA, Klein RL, Boeckman CR (1993) Gastroschisis: an 18-year review. J Pediatr Surg 28(5):650–652. https://doi.org/10.1016/0022-3468(93)90022-d
Poola AS, Aguayo P, Fraser JD et al (2019) Primary closure versus bedside silo and delayed closure for gastroschisis: a truncated prospective randomized trial. Eur J Pediatr Surg 29(2):203–208. https://doi.org/10.1055/s-0038-1627459
Hawkins RB, Raymond SL, St Peter SD et al (2020) Immediate versus silo closure for gastroschisis: results of a large multicenter study. J Pediatr Surg 55(7):1280–1285. https://doi.org/10.1016/j.jpedsurg.2019.08.002
Organization WH. Kenya Statistics (2019).
Organization WH. United Republic of Tanzania Statistics.
Organization WH. Malawi Statistics (2019)
Organization WH (2019). Uganda Statistics. https://doi.org/10.1213/ane.0000000000004363
Gajewski J, Pittalis C, Lavy C et al (2020) Anesthesia capacity of district-level hospitals in Malawi, Tanzania, and Zambia: a mixed-methods study. Anesth Analg 130(4):845–853. https://doi.org/10.1213/ANE.0000000000004363
Bustorff-Silva JM, Schmidt AF, Goncalves A, Marba S, Sbragia L (2008) The female condom as a temporary silo: a simple and inexpensive tool in the initial management of the newborn with gastroschisis. J Matern Fetal Neonatal Med 21(9):648–651. https://doi.org/10.1080/14767050802178003
Kusafuka J, Yamataka A, Okazaki T et al (2005) Gastroschisis reduction using “Applied Alexis”, a wound protector and retractor. Pediatr Surg Int 21(11):925–927. https://doi.org/10.1007/s00383-005-1518-2
Konig C, Simmen HP, Blaser J (1998) Bacterial concentrations in pus and infected peritoneal fluid–implications for bactericidal activity of antibiotics. J Antimicrob Chemother 42(2):227–232. https://doi.org/10.1093/jac/42.2.227
Nichols CRDJ, Pemberton PJ (1997) Rising incidence of gastroschisis in teenage pregnancies. J Maternal Fetal Med 6(4):225–229. https://doi.org/10.1002/(sici)1520-6661(199707/08)6:4%3C225::aid-mfm8%3E3.0.co;2-l
Davies MW, Kimble RM, Woodgate PG (2002) Ward reduction without general anaesthesia versus reduction and repair under general anaesthesia for gastroschisis in newborn infants. Cochrane Database Syst Rev 3:CD003671. https://doi.org/10.1002/14651858.CD003671
Elhosny A, Banieghbal B (2021) Simplified preformed silo bag crafted from standard equipment in African Hospitals. Afr J Paediatr Surg 18(2):123–126. https://doi.org/10.4103/ajps.AJPS_62_20
Acknowledgements
None.
Funding
Dr. Leraas’ work is supported by a T32 training grant in Surgical Oncology. BME-IDEA International Students Grants Program, VentureWell Grants; “Saving Intestines at Birth: Gastroschisis Silos for Sub-Saharan Africa (#20538-20).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Leraas, H.J., Biswas, A., Eze, A. et al. Low Cost Gastroschisis Silo for Sub-Saharan Africa: Testing in a Porcine Model. World J Surg 47, 545–551 (2023). https://doi.org/10.1007/s00268-022-06797-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06797-2