Abstract
Background
Gastrointestinal stromal tumors (GISTs) account for <1% of gastrointestinal cancers. The present study aimed to assess the outcomes of local and radical excision of non-metastatic rectal GISTs.
Methods
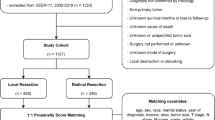
This study was a retrospective cohort analysis of patients with non-metastatic rectal GISTs in the NCDB. Patients were divided according to the surgical approach into local and radical excision and were compared in regard to the baseline characteristics and outcomes. A propensity-score matched analysis was performed to match the two groups for baseline confounders. The main outcomes were 5-year overall survival (OS), surgical margins, hospital stay, short-term mortality, and readmission.
Results
228 patients (54.8% male) with rectal GISTs were included. Before matching, 127 (55.7%) patients underwent local excision and 101 (44.3%) had radical excision. Patients who underwent local excision had more cT1-T2 and low-grade GISTs whereas patients who had radical excision received more neoadjuvant systemic treatment. After matching for clinical T stage, tumor grade, and neoadjuvant systemic therapy, 52 patients were included in each group. Local excision had a significantly higher rate of positive resection margins (42.2% vs. 19.1%, p = 0.02) and a shorter hospital stay (0 vs. 3 days, p < 0.001) than radical excision. The two groups had similar mean OS (139.8 vs. 133.1 months, p = 0.52).
Conclusions
Local excision was associated with a significantly higher incidence of positive resection margins and shorter hospital stay, yet similar overall survival to radical excision.


Similar content being viewed by others
References
PDQ Adult Treatment Editorial Board (2020) Gastrointestinal stromal tumors treatment (Adult) (PDQ®): Health Professional Version.
Miettinen M, Lasota J (2001) Gastrointestinal stromal tumors–definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch 438:1–12
Miettinen M, El-Rifai W, Sobin HL, Lasota J (2002) Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol 33:478–83
Kameyama H, Kanda T, Tajima Y et al (2018) Management of rectal gastrointestinal stromal tumor. Transl Gastroenterol Hepatol 3:8
Zhou Z, Chen Z, Chen M et al (2014) Clinicopathologic factors predicting outcomes in patients with gastrointestinal stromal tumors of the rectum and colon. Tumour Biol 35:4357–4362
Farid M, Lee MJ, Chew MH et al (2013) Localized gastrointestinal stromal tumor of the rectum: an uncommon primary site with prominent disease and treatment-related morbidities. Mol Clin Oncol 1:190–194
Eisenberg BL, Judson I (2004) Surgery and imatinib in the management of GIST: emerging approaches to adjuvant and neoadjuvant therapy. Ann Surg Oncol 11:465–475
Rutkowski P, Skoczylas J, Wisniewski P (2018) Is the surgical margin in gastrointestinal stromal tumors different? Visc Med 34:347–352
Centonze D, Pulvirenti E, Pulvirenti D’Urso A et al (2013) Local excision with adjuvant imatinib therapy for anorectal gastrointestinal stromal tumors. Tech Coloproctol 17:571–574
Demetri GD, von Mehren M, Blanke CD et al (2002) Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med 347:472–480
Nishida T, Shirao K, Sawaki A et al (2008) Efficacy and safety profile of imatinib mesylate (ST1571) in Japanese patients with advanced gastrointestinal stromal tumors: a phase II study (STI571B1202). Int J Clin Oncol 13:244–251
Wei J, Zhong J, Chen Z et al (2022) Survival outcome of local vs radical excision in rectal gastrointestinal stromal tumor: a SEER database analysis. BMC Surg 22:215
Hou YY, Lu SH, Zhou Y et al (2009) Stage and histological grade of gastrointestinal stromal tumors based on a new approach are strongly associated with clinical behaviors. Mod Pathol 22:556–569. https://doi.org/10.1038/modpathol.2009.11
Jakob J, Hohenberger P (2018) Neoadjuvant therapy to downstage the extent of resection of gastrointestinal stromal tumors. Visc Med 34(5):359–365. https://doi.org/10.1159/000493405
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates Publishers, Hillsdale
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458
Baik SH, Kim NK, Lee CH et al (2007) Gastrointestinal stromal tumor of the rectum: an analysis of seven cases. Surg Today 37:455–459
Choti MA (2022) Gastrointestinal stromal tumors (GISTs). Medscape. Available online at https://emedicine.medscape.com/article/278845-overview#a5.
Jakob J, Mussi C, Ronellenfitsch U et al (2013) Gastrointestinal stromal tumor of the rectum: results of surgical and multimodality therapy in the era of imatinib. Ann Surg Oncol 20:586–592
Wang T, Zhao Y, Wang M et al (2021) Radical resection versus local excision for low rectal gastrointestinal stromal tumor: a multicenter propensity score-matched analysis. Eur J Surg Oncol 47:1668–1674
Guo W, Yang Z, Wei Y et al (2020) Radical excision versus local resection for primary rectal gastrointestinal stromal tumors. Cohort Study Int J Surg 77:190–197
IJzerman NS, Mohammadi M, Tzanis D et al (2020) Quality of treatment and surgical approach for rectal gastrointestinal stromal tumour (GIST) in a large European cohort. Eur J Surg Oncol 46:1124–1130
Rutkowski P, Skoczylas J, Wisniewski P (2018) Is the surgical margin in gastrointestinal stromal tumors different? Visc Med 34(5):347–352. https://doi.org/10.1159/000491649
Shu P, Sun XF, Fang Y et al (2020) Clinical outcomes of different therapeutic modalities for rectal gastrointestinal stromal tumor: summary of 14-year clinical experience in a single center. Int J Surg 77:1–7
McCarter MD, Antonescu CR, Ballman KV et al (2012) Microscopically positive margins for primary gastrointestinal stromal tumors: analysis of risk factors and tumor recurrence. J Am Coll Surg 215:53–59
Gouveia AM, Pimenta AP, Capelinha AF, de la Cruz D, Silva P, Lopes JM (2008) Surgical margin status and prognosis of gastrointestinal stromal tumor. World J Surg 32:2375–2382
Singer S, Rubin BP, Lux ML et al (2002) Prognostic value of KIT mutation type, mitotic activity, and histologic subtype in gastrointestinal stromal tumors. J Clin Oncol 20:3898–3905
DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF (2000) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231:51–58
Laurent M, Brahmi M, Dufresne A et al (2019) Adjuvant therapy with imatinib in gastrointestinal stromal tumors (GISTs)-review and perspectives. Transl Gastroenterol Hepatol 4:24
Kumar A, Guss ZD, Courtney PT et al (2020) Evaluation of the use of cancer registry data for comparative effectiveness research. JAMA Netw Open 3(7):e2011985. https://doi.org/10.1001/jamanetworkopen.2020.11985
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46(3):399–424. https://doi.org/10.1080/00273171.2011.568786
Funding
SDW receives consulting fees for ARC/Corvus, Baxter, GI Supply, ICON Clinical Research Limited, Intuitive Surgical, Leading BioSciences/PalisadeBio, Livsmed, Medtronic, Stryker, Takeda and royalties from Intuitive Surgical, Karl Storz Endoscopy America Inc, Medtronic, Unique Surgical Innovations LLC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report any relevant financial disclosures or conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Emile, S.H., Horesh, N., Freund, M.R. et al. Outcomes of Local Excision Compared to Radical Excision of Rectal Gastrointestinal Stromal Tumors: A Propensity-Score Matched Analysis of the NCDB. World J Surg 47, 269–277 (2023). https://doi.org/10.1007/s00268-022-06778-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06778-5