Abstract
Background
Standard synthetic and biologic meshes, often used in hernia repair, have commonly been used and each have their strengths but associated drawbacks. Long-term biosynthetic absorbable (LTBA) mesh has been developed to combine the strengths of synthetic and biologic meshes without the associated weaknesses. As a newer type of mesh, the supporting evidence base is still growing, and their optimum use has yet to be defined. This consensus was initiated to provide insight into those situations where a LTBA might be considered the Standard of Care in ventral hernia repair grades 2–3 (original classification, 2010) of the Ventral Hernia Working Group.
Methods
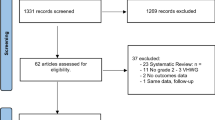
A steering group of expert surgeons identified 35 statements, based around the evidence supporting LTBA, surgical technique, patients type most suitable for LTBA, risk–benefit of LTBA, patient and surgeon considerations, LTBA value. Surgeons involved in hernia repair received an online survey to assess consensus with these statements. Consensus was defined as high if ≥ 70% and very high if ≥ 90% of respondents agreed. Statements that had not achieved consensus agreement were revised and these were then issued for a subsequent round. Finally, 34 statements were included.
Results
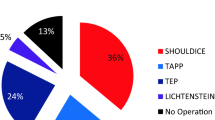
Two hundred fifty-five surgeons were involved. Fourteen statements (41%) achieved very high consensus, 24 achieved consensuses (≥ 70–< 90%), whilst one (3%) just failed to achieve consensus with an agreement score of 69%.
Conclusions
Expert consensus opinion about the use of LTBA for hernia (Grades 2–3) as the Standard of Care was achieved. Based on the consensus scores, the steering group derived eleven keys.



Similar content being viewed by others
References
Misiakos EP, Patapis P, Zavras N et al (2015) Current trends in laparoscopic ventral hernia repair. JSLS. 19(3):e201500048. https://doi.org/10.4293/JSLS.2015.00048
Brown CN, Finch JG (2010) Which mesh for hernia repair? Ann R Coll Surg Engl 92(4):272–278. https://doi.org/10.1308/003588410X12664192076296
FitzGerald JF, Kumar AS (2014) Biologic versus synthetic mesh reinforcement: what are the pros and cons? Clin Colon Rectal Surg 27(4):140–148. https://doi.org/10.1055/s-0034-1394155
Messa CA 4th, Kozak G, Broach RB et al (2019) When the mesh goes away: an analysis of poly-4-hydroxybutyrate mesh for complex hernia repair. Plast Reconstr Surg Glob Open 7(11):e2576. https://doi.org/10.1097/GOX.0000000000002576
Levy AS, Bogue JT, Morrison KA (2016) P4HB: the ideal mesh for complex abdominal wall reconstruction? Plast Reconstr Surg Glob Open 4(9 Suppl):116
Petro CC, Rosen MJ (2018) A current review of long-acting resorbable meshes in abdominal wall reconstruction. Plast Reconstr Surg 142(3 Suppl):84S-91S. https://doi.org/10.1097/PRS.0000000000004859
Rognoni C, Cuccurullo D, Borsoi L et al (2020) Clinical outcomes and quality of life associated with the use of a biosynthetic mesh for complex ventral hernia repair: analysis of the “Italian Hernia Club” registry. Sci Rep 10(1):10706. https://doi.org/10.1038/s41598-020-67821-w
Dalkey N, Helmer O (1963) An experimental application of the Delphi method to the use of experts. Manag Sci 9:458–467
Ventral Hernia Working Group, Breuing K, Butler CE et al (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148(3):544–558. https://doi.org/10.1016/j.surg.2010.01.008
Cobb WS, Carbonell AM, Kalbaugh CL et al (2009) Infection risk of open placement of intraperitoneal composite mesh. Am Surg. 75(9):762–7 (discussion 767–8)
Hawn MT, Snyder CW, Graham LA et al (2010) Long-term follow-up of technical outcomes for incisional hernia repair. J Am Coll Surg 210(5):648–55, 655–7. https://doi.org/10.1016/j.jamcollsurg.2009.12.038
Luijendijk RW, Hop WC, van den Tol MP et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343(6):392–398. https://doi.org/10.1056/NEJM200008103430603
Kokotovic D, Bisgaard T, Helgstrand F (2016) Long-term recurrence and complications associated with elective incisional hernia repair. JAMA 316(15):1575–1582. https://doi.org/10.1001/jama.2016.15217
Snyder CW, Graham LA, Gray SH et al (2011) Effect of mesh type and position on subsequent abdominal operations after incisional hernia repair. J Am Coll Surg. 212(4):496–502. https://doi.org/10.1016/j.jamcollsurg.2010.12.004 (discussion 502–4)
Deeken CR, Abdo MS, Frisella MM et al (2011) Physicomechanical evaluation of absorbable and nonabsorbable barrier composite meshes for laparoscopic ventral hernia repair. Surg Endosc 25(5):1541–1552. https://doi.org/10.1007/s00464-010-1432-0
Roth JS, Anthone GJ, Selzer DJ et al (2018) Prospective evaluation of poly-4-hydroxybutyrate mesh in CDC class I/high-risk ventral and incisional hernia repair: 18-month follow-up. Surg Endosc 32(4):1929–1936. https://doi.org/10.1007/s00464-017-5886-1
Martin DP, Badhwar A, Shah DV et al (2013) Characterization of poly-4-hydroxybutyrate mesh for hernia repair applications. J Surg Res 184(2):766–773. https://doi.org/10.1016/j.jss.2013.03.044
Singhal V, Szeto P, VanderMeer TJ et al (2012) Ventral hernia repair: outcomes change with long-term follow-up. JSLS 16(3):373–379. https://doi.org/10.4293/108680812X13427982377067
Buell JF, Sigmon D, Ducoin C et al (2017) Initial experience with biologic polymer scaffold (Poly-4-hydroxybuturate) in complex abdominal wall reconstruction. Ann Surg. 266(1):185–188. https://doi.org/10.1097/SLA.0000000000001916
Rosen MJ, Bauer JJ, Harmaty M et al (2017) Multicenter, prospective, longitudinal study of the recurrence, surgical site infection, and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh: The COBRA study. Ann Surg. 265(1):205–211. https://doi.org/10.1097/SLA.0000000000001601
Plymale MA, Davenport DL, Dugan A et al (2018) Ventral hernia repair with poly-4-hydroxybutyrate mesh. Surg Endosc. 32(4):1689–1694. https://doi.org/10.1007/s00464-017-5848-7
Keogh K, Slater K (2020) Comparison of biosynthetic versus synthetic mesh in clean and contaminated ventral hernia repairs. ANZ J Surg. 90(4):542–546. https://doi.org/10.1111/ans.15587
Abdelmoaty WF, Dunst CM, Filicori F et al (2020) Combination of surgical technique and bioresorbable mesh reinforcement of the crural repair leads to low early hernia recurrence rates with laparoscopic paraesophageal hernia repair. J Gastrointest Surg. 24(7):1477–1481. https://doi.org/10.1007/s11605-019-04358-y
Ruiz-Jasbon F, Ticehurst K, Ahonen J et al (2020) Results at 3-year follow-up of totally extraperitoneal (TEP) hernia surgery with long-term resorbable mesh. Hernia 24:669–676. https://doi.org/10.1007/s10029-019-02116-2
van Rooijen MMJ, Jairam AP, Tollens T et al (2018) A post-market, prospective, multi-center, single-arm clinical investigation of Phasix™ mesh for VHWG grade 3 midline incisional hernia repair: a research protocol. BMC Surg. 18(1):104. https://doi.org/10.1186/s12893-018-0439-7
Bueno-Lledó J, Ceno M, Perez-Alonso C et al (2021) Biosynthetic resorbable prosthesis is useful in single-stage management of chronic mesh infection after abdominal wall hernia repair. World J Surg. 45(2):443–450. https://doi.org/10.1007/s00268-020-05808-4
Charleux-Muller D, Hurel R, Fabacher T et al (2021) Slowly absorbable mesh in contaminated incisional hernia repair: results of a French multicenter study. Hernia 25(4):1051–1059. https://doi.org/10.1007/s10029-020-02366-5
Roth JS, Anthone GJ, Selzer DJ et al (2020) Prospective, multicenter study of P4HB (Phasix™) mesh for hernia repair in cohort at risk for complications: 3-Year follow-up. Ann Med Surg (Lond). 61:1–7. https://doi.org/10.1016/j.amsu.2020.12.002
Vauclair E, Bert M, Facy O et al (2021) What results can be expected one year after complex incisional hernia repair with biosynthetic mesh? J Visc Surg. 158(2):111–117. https://doi.org/10.1016/j.jviscsurg.2020.07.008
Funding
This project was funded by BD Medical Ltd by supporting the costs of methodological process, which was performed by Triducive Partners Limited. Ian Walker and Tim Warren worked with Triducive Partners Limited and acted as independent facilitators during the expert group discussions to identify key topics and to capture the expert consensus statements. The survey distribution and analysis of results were performed by the experts and remained anonymous and independent.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Morales-Conde Salvador, Berrevoet Frederick, Lars Nannestad Jorgensen, Marchi Domenico, Ortega-Deballon Pablo, and Windsor Alistair have no conflicts of interest or financial ties to disclose.
Ethical standard
The present study was approved by our institutional review board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morales-Conde, S., Berrevoet, F., Jorgensen, L.N. et al. Establishing Peer Consensus About the Use of Long-Term Biosynthetic Absorbable Mesh for Hernia (Grades 2–3) as the Standard of Care. World J Surg 46, 2996–3004 (2022). https://doi.org/10.1007/s00268-022-06743-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06743-2