Abstract
Background
Due to duty hour regulations, patient safety and inadequate operative time simulation have become a necessary part of surgical education and training in residency. Currently, there is no formal adoption of simulators for the use of surgical education or assessment in hand surgery. This literature review analyzes that the simulation techniques established thus far in hand surgery.
Methods
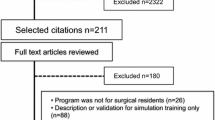
A comprehensive literature search was performed on PubMed. Search results were filtered by title and abstract to isolate articles that were relevant to simulation in hand surgery. Articles that were nonspecific to the hand, non-English and cadaveric were excluded. Additional articles were identified through references from the initial search.
Results
A total of 1192 articles were yielded from the initial query. After the application of the inclusion criteria, this was narrowed down to 28 articles. Another 8 additional articles were excluded as they did not pertain to the hand although the simulators could be adapted for hand surgery. A total of 20 articles were included in this study.
Conclusions
Surgical simulation is a growing and essential field of surgical education. Simulators in hand surgery are limited and require further research and validation. Like other surgical subspecialties, hand surgery may benefit from the adoption of an official simulation curriculum for the assessment of residents and enhancement of technical skills.




Similar content being viewed by others
References
ACGME https://www.acgme.org/What-We-Do/Accreditation/Clinical-Experience-and-Education-formerly-Duty-Hours/History-of-Duty-Hours. Accessed
Philibert I, Nasca T, Brigham T, Shapiro J (2013) Duty-hour limits and patient care and resident outcomes: can high-quality studies offer insight into complex relationships? Annu Rev Med 64:467–483
Carlin AM, Gasevic E, Shepard AD (2007) Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg 193(3):326–329
Thomas MP (2013) The role of simulation in the development of technical competence during surgical training: a literature review. Int J Med Educ 4:48–58
Ziv A, Small SD, Wo PR (2000) Patient safety and simulation-based medical education. Med Teach 22(5):489–495
Agha RA, Fowler AJ (2015) The role and validity of surgical simulation. Int Surg 100(2):350–357
Bradley P (2006) The history of simulation in medical education and possible future directions. Med Educ 40(3):254–262
Badash I, Burtt K, Solorzano CA, Carey JN (2016) Innovations in surgery simulation: a review of past, current and future techniques. Ann Transl Med 4:453
Massoth C, Röder H, Ohlenburg H et al (2019) High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ. https://doi.org/10.1186/s12909-019-1464-7
Kneebone RL, Kidd J, Nestel D et al (2005) Blurring the boundaries: scenario-based simulation in a clinical setting. Med Educ 39(6):580–587
Surgery TABo. General Requirments for Board Certification. http://www.absurgery.org/default.jsp?certhandce. Accessed
Rhodes ND, Wilson PA, Southern SJ (2001) The flexor-tendon repair simulator. Br J Plast Surg 54:373–374
Hoeyberghs JL, Flemming AFS (1994) Flexor tendon repair in perfect safety. Eur J Plast Surg 17(4):215–217
Tare M (2004) Dental rolls: a suitable model for practising tendon repair techniques. J Hand Surg Br 29(5):506–507
Juma AM, Vuppalapati G, Martin J (2004) A see-through in vitro tendon repair model. Plast Reconstr Surg 113(3):1097–1098
Wright TC, Widdowson D, Khan M, Tiernan E, Hormbrey E (2006) A cost-effective training tool for flexor tendon repair: pig’s trotters. J Plast Reconstr Aesthet Surg 59(1):107–108
Kamath J, Chandra G, Kamath R, Kumar A, Bhardwaj P (2009) Flexor tendon repair simulator. Tech Hand Up Extrem Surg 13:117–118
Ingraham JM, Weber RA (2009) Utilizing a simulated tendon to teach tendon repair technique. Hand (N Y). 4:150–155
Hasham S, Khandwala A, Southern SJ (2005) Soft-tissue simulator: helping trainees with fracture fixation. Plast Reconstr Surg 115:957
Brichacek M, Diaz-Abele J, Shiga S, Petropolis C (2018) Three-dimensional printed surgical simulator for Kirschner wire placement in hand fractures. Plast Reconstr Surg Glob Open 6(3):e1706
Wu YY, Rajaraman M, Guth J et al (2018) A high-fidelity tactile hand simulator as a training tool to develop competency in percutaneous pinning in residents. J Am Acad Orthop Surg Glob Res Rev 2(7):e028
Maier J, Weiherer M, Huber M, Palm C (2019) Imitating human soft tissue on basis of a dual-material 3D print using a support-filled metamaterial to provide bimanual haptic for a hand surgery training system. Quant Imaging Med Surg 9:30–42
Lazarus P, Pire E, Sapa C et al (2017) Design and evaluation of a new synthetic wrist procedural simulator (Wristsim((R))) for training of distal radius fracture fixation by volar plating. Hand Surg Rehabil 36(4):275–280
Naroura I, Hidalgo Diaz JJ, Xavier F et al (2018) Teaching of distal radius shortening osteotomy: three-dimensional procedural simulator versus bone procedural simulator. J Hand Surg Eur 43(9):961–966
Obdeijn MC, Alewijnse JV, Mathoulin C, Liverneaux P, Tuijthof GJ, Schijven MP (2014) Development and validation of a computer-based learning module for wrist arthroscopy. Chir Main 33(2):100–105
Computer-Based Training System for Simulating Wrist Arthroscopy (2008) IEEE conference publication. IEEE. https://ieeexplore.ieee.org/document/4562028. Published 2008. Accessed
Zemirline A, Agnus V, Soler L, Mathoulin CL, Obdeijn M, Liverneaux PA (2013) Augmented reality-based navigation system for wrist arthroscopy: feasibility. J Wrist Surg 2(4):294–298
CLA. Arthroscopic Model Of The Wrist. https://www.gtsimulators.com/CLA-Arthroscopic-Model-of-the-Wrist-p/cla16.htm. Accessed
Amer KM, Mur T, Amer K, Ilyas AM (2017) A mobile-based surgical simulation application: a comparative analysis of efficacy using a carpal tunnel release module. J Hand Surg Am 42(5):389.e381-389.e389
Tulipan J, Miller A, Park AG, Labrum JT, Ilyas AM (2019) Touch surgery: analysis and assessment of validity of a hand surgery simulation “App.” Hand (N Y). 14(3):311–316
Paro JAM, Luan A, Lee GK (2017) Validation of a cognitive task simulation and rehearsal tool for open carpal tunnel release. Arch Plast Surg 44(3):223–227
de Montbrun SL, MacRae H (2012) Simulation in surgical education. Clin Colon Rectal Surg 25:156–165
Shah S, Wain R, Syed S (2010) A novel training model for nerve repair. Ann R Coll Surg Engl 92(3):260
Kamath J, Jayasheelan N, Sujir P (2017) A simulator for nerve repair. J Hand Surg Eur 42(9):960–961
Meyer-Marcotty MV, Redeker J, Herold C, Busch KH, Rennekampff HO, Vogt PM (2008) A flap simulator for training in local defect coverage. Chirurg 79(12):1141–1144
Chan WY, Matteucci P, Southern SJ (2007) Validation of microsurgical models in microsurgery training and competence: a review. Microsurgery 27(5):494–499
Evgeniou E, Walker H, Gujral S (2018) The role of simulation in microsurgical training. J Surg Educ 75(1):171–181
Hafford ML, Van Sickle KR, Willis RE et al (2013) Ensuring competency: are fundamentals of laparoscopic surgery training and certification necessary for practicing surgeons and operating room personnel? Surg Endosc 27(1):118–126
Vassiliou MC, Dunkin BJ, Fried GM et al (2014) Fundamentals of endoscopic surgery: creation and validation of the hands-on test. Surg Endosc 28(3):704–711
Funding
This study was supported in part by the Mayo Clinic Center for Individualized Medicine and the Mayo Clinic Center for Regenerative Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Declaration of HELSINKI 1975, as revised in 2008.
Informed Consent
Informed consent was not obtained due to the type of this study (systematic literature review).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saleem, H.Y., Kaplan, J.L., Torres-Guzman, R.A. et al. Simulation in Hand Surgery: A Literature Review. World J Surg 46, 718–724 (2022). https://doi.org/10.1007/s00268-021-06400-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06400-0