Abstract
Background
This research adopted a care protocol from high-income countries in a level II/III hospital in a middle-income country to decrease morbidity and mortality associated with gastroschisis.
Methods
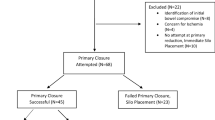
We established a multidisciplinary protocol to treat patients with gastroschisis prospectively from November 2012 to November 2018. This included prenatal diagnosis, presence of a neonatologist and pediatric surgeon at birth, and either performing primary closure on the patients with an Apgar score of 8/9, mild serositis, and no breathing difficulty or placing a preformed silo, when unable to fulfill these criteria, under sedation and analgesia (no intubation) in the operating room or at the patients’ bedside. The subsequent management took place in the neonatal intensive care unit. The data were analyzed through the Mann–Whitney and Student’s t-distribution for the two independent samples; the categorical variables were analyzed through a chi-square distribution or Fisher’s exact test.
Results
In total, 55 patients were included in the study: 33 patients (60%) were managed with a preformed silo, whereas 22 patients (40%) underwent primary closure. Prenatal diagnosis (P = 0.02), birth at the main hospital (P = 0.02), and the presence of a pediatric surgeon at birth (P = 0.04) were associated with successful primary closure. The primary closure group had fewer fasting days (P < 0.001) and a shorter neonatal intensive care unit length of stay (P = 0.025). The survival rate was 92.7% (51 patients).
Conclusion
The treatment model modified to fit the means of our hospital proved successful.




Similar content being viewed by others
References
Sheriff E (2018) Surgical strategies in complex gastroschisis. Semin Pediatr Surg 27(5):309–315. https://doi.org/10.1053/j.sempedsurg.2018.08.003
Bergholz R, Boettcher M, Reinshagen K, Wenke K (2014) Complex gastroschisis is a different entity to simple gastroschisis affecting morbidity and mortality: a systematic review and meta-analysis. J Pediatr Surg 49:1527–1532. https://doi.org/10.1016/J.JPEDSURG.2014.08.001
Wright NJ (2019) Management and outcomes of gastrointestinal congenital anomalies in low, middle and high income countries: protocol for a multicentre, international, prospective cohort study. BMJ Open 9:e030452. https://doi.org/10.1136/bmjopen-2019-030452
International Clearinghouse for Birth Defects Surveillance and Research Annual Report (2012) The international center on birth defects: ICBDSR centre [ISSN: 0743–5703]
Salinas-Torres VM, Salinas-Torres RA, Cerda-Flores RM, Martínez-de-Villarreal LE (2018) Prevalence, mortality, and spatial distribution of gastroschisis in Mexico. J Pediatr Adolesc Gynecol. https://doi.org/10.1016/j.jpag.2017.12.013
Davila-Zalles C, Peñarrieta-Daher A, Bracho-Blanchet E et al (2018) A Gastroschisis bundle: effect of a quality improvement protocol on morbidity and mortality. J Pediatr Surg 53:2117–2122
Ross AR, Eaton S, Zani A, Ade-Ajayi N, Pierro A, Hall NJ (2015) The role of preformed silos in the management of infants with gastroschisis: a systematic review and meta-analysis. Pediatr Surg Int 31:473–483
Allotey J, Davenport M, Njere I et al (2007) Benefit of preformed silos in the management of gastroschisis. Pediatr Surg Int 23:1065–1069
Pastor AC, Phillips JD, Fenton SJ et al (2008) Routine use of a SILASTIC spring-loaded silo for infants with gastroschisis: a multicentre randomized controlled trial. J Pediatr Surg 43:1807–1812
Kunz SN, Tieder JS, Whitlock KJ, Jackson C, Avansino JR (2013) Primary fascial closure versus staged closure with silo in patients with gastroschisis: a meta-analysis. J Pediatr Surg 48:845–857
Ogasawara Y, Okazaki T, Kato Y et al (2009) Spontaneous sutureless closure of the abdominal wall defect in gastroschisis using a commercial wound retractor system. Pediatr Surg Int 25:973–976
Sandler A, Lawrence J, Meehan J, Phearman L, Soper R (2004) A“plasti” sutureless abdominal wall closure in gastroschisis. J Pediatr Surg 39:738–741
Bianchi A, Dickson AP, Alizai NK (2002) Elective delayed midgut reduction-no anesthesia for gastroschisis: selection and conversion criteria. J Pediatr Surg 37:1334–1336
Kimble RM, Singh SJ, Bourke C et al (2001) Gastroschisis reduction under analgesia in the neonatal unit. J Pediatr Surg 36:1672–1674
Blankenship SA, Brown KE, Simon LE, Stout MJ, Tuuli MG (2020) Antenatal corticosteroids in preterm small-for-gestational age infants: a systematic review and meta-analysis. Am J Obstet Gynecol MFM 2(4):100215. https://doi.org/10.1016/j.ajogmf.2020.100215
Cowan KN, Puligandla PS, Laberge J-M et al (2012) The gastroschisis prognostic score: reliable outcome prediction in gastroschisis. J Pediatr Surg 47:1111–1117. https://doi.org/10.1016/j.jpedsurg.2012.03.010
Oakes MC, Porto M, Chung JH (2018) Advances in prenatal and perinatal diagnosis and management of gastroschisis. Semin Pediatr Surg. https://doi.org/10.1053/j.sempedsurg.2018.08.006
Petrosyan P, Sandler AD (2018) Closure methods in gastroschisis. Semin Pediatr Surg. https://doi.org/10.1053/j.sempedsurg.2018.08.009
Wright NJ, Sekabira J, Ade-Ajayi N (2018) Care of infants with gastroschisis in low-resource settings. Semin Pediatr Surg. https://doi.org/10.1053/j.sempedsurg.2018.08.004
Global PaedSurg Research Collaboration (2021) Mortality from gastrointestinal congenital anomalies at 264 hospitals in 74 low-income, middle-income, and high-income countries: a multicentre, international, prospective cohort study. Lancet 398(10297):325–339. https://doi.org/10.1016/S0140-6736(21)00767-4
Egger PA, de Souza MP, Riedo CO, Dutra AC, da Silva MT, Pelloso SM, Carvalho MBD (2021) Gastroschisis annual incidence, mortality and trends in extreme Southern Brasil. J Pediatr (Rio J). https://doi.org/10.1016/j.jped.2021.04.007
Martins MR, Abreu I, Meio MD et al (2020) Gastroschisis in the neonatal period: a prospective case-series in a Brazilian referral center. J Pediatr Surg 55:1546–1551. https://doi.org/10.1016/j.jpedsurg.2020.04.011
Kirollos DW, Abdel-Latif ME (2017) Mode of delivery and outcomes of infants with gastroschisis: a meta-analysis of observational studies. Arch Dis Child Fetal Neonatal Ed. https://doi.org/10.1136/archdischild-2016-312394
Segel SY, Marder SJ, Parry S et al (2001) Fetal abdominal wall defects and mode of delivery: a systematic review. Obstet Gynecol 98:867–873
Fullerton BS, Velazco CS, Sparks EA et al (2017) Contemporary outcomes of infants with gastroschisis in North America: a multicenter cohort study. J Pediatr 188:192-197.e6. https://doi.org/10.1016/j.jpeds.2017.06.013
Gurien LA, Dassinger MS, Burford JM, Saylors ME, Smith SD (2017) Does timing of gastroschisis repair matter? A comparison using the ACS NSQIP pediatric database. J Pediatr Surg 52:1751–1754
Acknowledgments
We would like to express our sincere gratitude to Dr. Juan-Carlos Duarte-Valencia for his assistance in writing the protocol, Lourdes Velasco-Vazquez for the statistical analysis, Aurora Aramburo-Papayanopulos for the writing of this study, and Mr. Joel Ayala-Huerta and Francisco Barajas-Martinez for collating all the records.
Funding
No funding was secured for this study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Informed consent
Was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Escarcega-Fujigaki, P., Hernandez-Peredo-Rezk, G., Wright, N.J. et al. Gastroschisis: A Successful, Prospectively Evaluated Treatment Model in a Middle-Income Country. World J Surg 46, 322–329 (2022). https://doi.org/10.1007/s00268-021-06357-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06357-0