Abstract
Background
Minimally invasive distal pancreatectomy (MIDP) is being adopted increasingly worldwide. This study aimed to compare the short-term outcomes of patients who underwent MIDP versus open distal pancreatectomy (ODP).
Methods
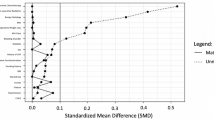
A retrospective review of all patients who underwent a DP in our institution between 2005 and 2019 was performed. Propensity score matching based on relevant baseline factors was used to match patients in the ODP and MIDP groups in a 1:1 manner. Outcomes reported include operative duration, blood loss, postoperative length of stay, morbidity, mortality, postoperative pancreatic fistula rates, reoperation and readmission.
Results
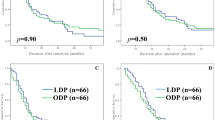
In total, 444 patients were included in this study. Of 122 MIDP patients, 112 (91.8%) could be matched. After matching, the median operating time for MIDP was significantly longer than ODP [260 min (200–346.3) vs 180 (135–232.5), p < 0.001], while postoperative stay for MIDP was significantly shorter [median 6 days (5–8) versus 7 days (6–9), p = 0.015]. There were no significant differences noted in any of the other outcomes measured. Over time, we observed a decrease in the operation times of MIDP performed at our institution.
Conclusion
Adoption of MIDP offers advantages over ODP in terms of a shorter postoperative hospital stay, without an increase in morbidity and/or mortality but at the expense of a longer operation time.

Similar content being viewed by others
References
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8(5):408–410
Tran Cao HS, Lopez N, Chang DC et al (2014) Improved perioperative outcomes with minimally invasive distal pancreatectomy: results from a population-based analysis. JAMA Surg 149(3):237–243
Goh BK, Chan CY, Soh HL et al (2017) A comparison between robotic-assisted laparoscopic distal pancreatectomy versus laparoscopic distal pancreatectomy. Int J Med Robot. 13(1):e1733
Aggarwal R, Hance J, Darzi A (2004) Robotics and surgery: a long-term relationship? Int J Surg 2(2):106–109
Köckerling F (2014) Robotic vs. standard laparoscopic technique–what is better? Front Surg 1:15
Lof S, van der Heijde N, Abuawwad M et al (2021) Robotic versus laparoscopic distal pancreatectomy: multicentre analysis. Br J Surg 108(2):188–195
Chung JC, Kim HC, Song OP (2014) Laparoscopic distal pancreatectomy for benign or borderline malignant pancreatic tumors. Turk J Gastroenterol 25(Suppl 1):162–166
Huang J, Yadav DK, Xiong C, Sheng Y, Zhou X, Cai X (2019) Laparoscopic spleen-preserving distal pancreatectomy (lspdp) versus open spleen-preserving distal pancreatectomy (OSPDP): a comparative study. Can J Gastroenterol Hepatol 2019:9367868
Limongelli P, Belli A, Russo G et al (2012) Laparoscopic and open surgical treatment of left-sided pancreatic lesions: clinical outcomes and cost-effectiveness analysis. Surg Endosc 26(7):1830–1836
Mehta SS, Doumane G, Mura T, Nocca D, Fabre JM (2012) Laparoscopic versus open distal pancreatectomy: a single-institution case-control study. Surg Endosc 26(2):402–407
Stauffer JA, Coppola A, Mody K, Asbun HJ (2016) Laparoscopic versus open distal pancreatectomy for pancreatic adenocarcinoma. World J Surg 40(6):1477–1484
Vijan SS, Ahmed KA, Harmsen WS et al (2010) Laparoscopic vs open distal pancreatectomy: a single-institution comparative study. Arch Surg 145(7):616–621
de Rooij T, van Hilst J, van Santvoort H et al (2019) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg 269(1):2–9
Björnsson B, Larsson AL, Hjalmarsson C, Gasslander T, Sandström P (2020) Comparison of the duration of hospital stay after laparoscopic or open distal pancreatectomy: randomized controlled trial. Br J Surg 107(10):1281–1288
Lyu Y, Cheng Y, Wang B, Zhao S, Chen L (2020) Comparison of 3 minimally invasive methods versus open distal pancreatectomy: a systematic review and network meta-analysis. Surg Laparosc Endosc Percutan Tech 31(1):104–112
Kwon, J., S.Y. Park, Y. Park, et al. (2020). A comparison of minimally invasive vs open distal pancreatectomy for resectable pancreatic ductal adenocarcinoma: Propensity score matching analysis. J Hepatobiliary Pancreat Sci.
Raoof M, Ituarte PHG, Woo Y et al (2018) Propensity score-matched comparison of oncological outcomes between laparoscopic and open distal pancreatic resection. Br J Surg 105(5):578–586
van Hilst J, de Rooij T, Klompmaker S et al (2019) Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a pan-european propensity score matched study. Ann Surg 269(1):10–17
Nakamura M, Wakabayashi G, Miyasaka Y et al (2015) Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepatobiliary Pancreat Sci 22(10):731–736
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Hartwig W, Vollmer CM, Fingerhut A et al (2014) Extended pancreatectomy in pancreatic ductal adenocarcinoma: definition and consensus of the international study group for pancreatic surgery (ISGPS). Surgery 156(1):1–14
International Agency for Research on Cancer, World Health Organization, and International Academy of Pathology, Digestive system tumours. 5 ed, ed. D.E. Elder. Vol. 1. 2019: IARC.
Austin PC (2008) A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med 27(12):2037–2049
Nakamura M, Nakashima H (2013) Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? a meta-analysis of laparoscopic pancreatectomy. J Hepatobiliary Pancreat Sci 20(4):421–428
Nigri GR, Rosman AS, Petrucciani N et al (2011) Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc 25(5):1642–1651
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255(6):1048–1059
Gavriilidis P, Roberts KJ, Sutcliffe RP (2019) Comparison of robotic vs laparoscopic vs open distal pancreatectomy A systematic review and network meta-analysis. HPB (Oxford) 21(10):1268–1276
Lyu, Y., Y. Cheng, B. Wang, S. Zhao, and L. Chen (2020). Assessment of laparoscopic versus open distal pancreatectomy: a systematic review and meta-analysis. Minim Invasive Ther Allied Technol 1–9.
van Hilst J, de Graaf N, Abu Hilal M, Besselink MG (2021) The landmark series: minimally invasive pancreatic resection. Ann Surg Oncol 28(3):1447–1456
Riviere D, Gurusamy KS, Kooby DA et al (2016) Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Database Syst Rev 4(4):Cd011391
Lee SQ, Kabir T, Koh YX et al (2020) A single institution experience with robotic and laparoscopic distal pancreatectomies. Ann Hepatobiliary Pancreat Surg 24(3):283–291
Goh BKP, Zeng G, Low TY, Chua DW, Koh YX, Lim KI (2020) Changing trends and outcomes associated with the adoption of minimally-invasive pancreato-biliary surgery: Contemporary experience of a “self-taught” early adopter in Southeast Asia. J Minim Access Surg 16(4):341–347
Chan, K.S., Z.K. Wang, N. Syn, and B.K.P. Goh, Learning curve of laparoscopic and robotic pancreas resections: a systematic review. Surgery, 2021.
Goh BKP, Lee SY, Kam JH et al (2018) Evolution of minimally invasive distal pancreatectomies at a single institution. J Minim Access Surg 14(2):140–145
Søreide K, Olsen F, Nymo LS, Kleive D, Lassen K (2019) A nationwide cohort study of resection rates and short-term outcomes in open and laparoscopic distal pancreatectomy. HPB (Oxford) 21(6):669–678
Goh BK, Teo RY (2020) Current status of laparoscopic and robotic pancreatic surgery and its adoption in Singapore. Ann Acad Med Singap 49(6):377–383
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raghupathy, J., Lee, CY., Huan, S.K.W. et al. Propensity-Score Matched Analyses Comparing Clinical Outcomes of Minimally Invasive Versus Open Distal Pancreatectomies: A Single-Center Experience. World J Surg 46, 207–214 (2022). https://doi.org/10.1007/s00268-021-06306-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06306-x