Abstract
Purpose
To mitigate intraoperative adverse events, it is important to understand the context in which these errors occur. The purpose of this study is to characterize the IAEs and potential distractions that occur in minimally invasive urologic procedures.
Methods
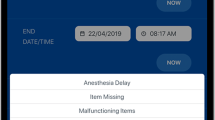
We conducted a prospective cohort study in patients undergoing laparoscopic urologic surgery at an academic health center. The OR Black Box, a unique technology system which captures video and audio recordings of the operating room as well as the operative field, was used to collect data regarding procedure type, critical step, IAEs, and distractions.
Results
Of a total of 80 cases analyzed, the majority of these cases were partial nephrectomy (n = 36; 45%), radical nephrectomy (n = 20; 25%), and adrenalectomy (n = 4; 5%). Across all cases, there were a total of 138 clinically significant IAEs, 10 of which (14%) were of the highest severity (five on the SEVerity of intraoperative Events and Rectification Tool (SEVERE) matrix). Of these, 70 (51%) occurred during an a priori defined critical step of the operation. Distractions were common across all cases. The median rate of external communication per case was 16 events (IQR 11-22); and per critical step was 4 (IQR 2.75-8), while median room traffic per case was 65 entries/exits (IQR 42-76); and per critical step was 17 (IQR 10-65).
Conclusion
Our data demonstrate that IAEs occur frequently during all phases of the operation at hand. Future study will be required to examine the role of distractions and IAE as well as IAE and their relationship to post-operative clinical outcomes.



Similar content being viewed by others
References
de Zegers M, BMC. (2011) The incidence, root-causes, and outcomes of adverse events in surgical. Patient Saf Surg. 5(13):1–11
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Wojcik BM, Han K, Peponis T, Velmahos G, Kaafarani HMA (2019) Impact of intra-operative adverse events on the risk of surgical site infection in abdominal surgery. Surg Infect (Larchmt) 20(3):174–183. https://doi.org/10.1089/sur.2018.157
Yoon RS, Alaia MJ, Hutzler LH, Bosco JA (2015) Using “near misses” analysis to prevent wrong-site surgery. J Healthc Qual. https://doi.org/10.1111/jhq.12037
Jung JJ, Adams-McGavin RC, Grantcharov TP (2019) Underreporting of veress needle injuries: comparing direct observation and chart review methods. J Surg Res 236:266–270. https://doi.org/10.1016/j.jss.2018.11.039
Weigl M, Müller A, Vincent C, Angerer P, Sevdalis N (2012) The association of workflow interruptions and hospital doctors’ workload: a prospective observational study. BMJ Qual Saf 21(5):399–407. https://doi.org/10.1136/bmjqs-2011-000188
Sevdalis N, Undre S, McDermott J, Giddie J, Diner L, Smith G (2014) Impact of intraoperative distractions on patient safety: a prospective descriptive study using validated instruments. World J Surg 38(4):751–758. https://doi.org/10.1007/s00268-013-2315-z
Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM (2007) Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery 142(5):658–665. https://doi.org/10.1016/j.surg.2007.07.034
Healey AN, Primus CP, Koutantji M (2007) Quantifying distraction and interruption in urological surgery. Qual Saf Heal Care 16(2):135–139. https://doi.org/10.1136/qshc.2006.019711
Goldenberg MG, Jung J, Grantcharov TP (2017) Using data to enhance performance and improve quality and safety in surgery. JAMA Surg 152(10):972–973. https://doi.org/10.1001/jamasurg.2017.2888
Sevdalis N, Forrest D, Undre S, Darzi A, Vincent C (2008) Annoyances, disruptions, and interruptions in surgery: the Disruptions in Surgery Index (DiSI). World J Surg. https://doi.org/10.1007/s00268-008-9624-7
Bonrath EM, Zevin B, Dedy NJ, Grantcharov TP (2013) Error rating tool to identify and analyse technical errors and events in laparoscopic surgery. British J Surg. https://doi.org/10.1002/bjs.9168
Jung JJ, Grantcharov TP (2019) Development and evaluation of a novel instrument to measure severity of intraoperative events using video data. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2019.08.328
Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G (2013) Development of a behavioural marker system for scrub practitioners’ non-technical skills (SPLINTS system). J Eval Clin Pract. https://doi.org/10.1111/j.1365-2753.2012.01825.x
Yule S, Flin R, Maran N, Rowley D, Youngson G, Paterson-Brown S (2008) Surgeons’ non-technical skills in the operating room: Reliability testing of the NOTSS behavior rating system. World J Surg. https://doi.org/10.1007/s00268-007-9320-z
Flin R, Patey R (2011) Non-technical skills for anaesthetists: developing and applying ANTS. Best Pract Res Clin Anaesthesiol. https://doi.org/10.1016/j.bpa.2011.02.005
Greenberg CC (2009) Learning from adverse events and near misses. J Gastrointest Surg. https://doi.org/10.1007/s11605-008-0693-6
Kashiwazaki D, Saito H, Uchino H, et al. Morbidity and Mortality Conference Can Reduce Avoidable Morbidity in Neurosurgery: Its Educational Effect on Residents and Surgical Safety Outcomes. In: World Neurosurgery. ; 2020. doi:https://doi.org/10.1016/j.wneu.2019.09.018
Haynes AB, Weiser TG, Berry WR et al (2009) A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. https://doi.org/10.1056/NEJMsa0810119
Kapoor A, Siemens DR (2014) “I told you so”: examining the impact of the surgical safety checklist. Can Urol Assoc J. https://doi.org/10.5489/cuaj.2079
Chen C, White L, Kowalewski T et al (2014) Crowd-sourced assessment of technical skills: a novel method to evaluate surgical performance. J Surg Res. https://doi.org/10.1016/j.jss.2013.09.024
Van Hove PD, Tuijthof GJM, Verdaasdonk EGG, Stassen LPS, Dankelman J (2010) Objective assessment of technical surgical skills. Br J Surg. https://doi.org/10.1002/bjs.7115
Goldenberg MG, Elterman D (2019) From box ticking to the black box: the evolution of operating room safety. World J Urol. https://doi.org/10.1007/s00345-019-02886-5
Statement on Distractions in the Operating Room. https://www.facs.org/about-acs/statements/89-distractions. Accessed April 7, 2020.
Feuerbacher RL, Funk KH, Spight DH, Diggs BS, Hunter JG (2012) Realistic distractions and interruptions that impair simulated surgical performance by novice surgeons. Arch Surg. https://doi.org/10.1001/archsurg.2012.1480
Suh IH, Chien JH, Mukherjee M, Park SH, Oleynikov D, Siu KC (2010) The negative effect of distraction on performance of robot-assisted surgical skills in medical students and residents. Int J Med Robot Comput Assist Surg. https://doi.org/10.1002/rcs.338
Jung JJ, Jüni P, Lebovic G, Grantcharov T (2020) First-year Analysis of the Operating Room Black Box Study. Ann Surg. https://doi.org/10.1097/SLA.0000000000002863
Birkmeyer JD, Finks JF, O’Reilly A et al (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med. https://doi.org/10.1056/NEJMsa1300625
Acknowledgements
Surgical Safety Technologies aided in the collection and analysis of the data as all data are centralized with their team post-collection in the operating room. In particular, we acknowledge Vanessa Palter, MD, Stephen Townsend, Daisy De La Cruz, Adolfo Rios, and Juliano Montes for their assistance in OBB setup and data analysis.
Funding
No grant funding was required for this research.
Author information
Authors and Affiliations
Contributions
AR contributed to data collection, data analysis, manuscript writing/editing, LB contributed to data analysis, manuscript editing, TA contributed to manuscript editing, MJ contributed to protocol development, manuscript editing, and LK contributed to protocol development, data collection, manuscript editing.
Corresponding author
Ethics declarations
Conflicts of interest
All of the others declare no conflicts of interests.
Ethics approval
This study was covered under an institutional quality improvement initiative and waived the need for participation or publication consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rai, A., Beland, L., Aro, T. et al. Patient Safety in the Operating Room During Urologic Surgery: The OR Black Box Experience. World J Surg 45, 3306–3312 (2021). https://doi.org/10.1007/s00268-021-06251-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06251-9