Abstract
Background
Prediction of failure of nonoperative management (NOM) in uncomplicated appendicitis (UA) is difficult. This study aimed to establish a new prediction model for NOM failure in UA.
Methods
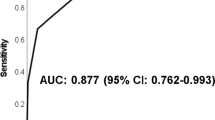
We included 141 adults with UA who received NOM as initial treatment. NOM failure was defined as conversion to operation during hospitalization. Independent predictors of NOM failure were identified using logistic regression analysis. A prediction model was established based on these independent predictors. Receiver operating characteristic (ROC) curve analysis and the Hosmer–Lemeshow test were used to assess the discrimination and calibration of the model, respectively, and risk stratification using the model was performed.
Results
Among 141 patients, NOM was successful in 120 and unsuccessful in 21. Male sex, maximal diameter of the appendix, and the presence of fecalith were identified as independent predictors of NOM failure for UA. A prediction model with scores ranging from 0 to 3 was established using the three variables (male sex, maximal diameter of the appendix ≥ 15 mm, and the presence of fecalith). The area under the ROC curve for the new prediction model was 0.778, and the model had good calibration (P = 0.476). A score of 2 yielded a sensitivity of 71.4% and a specificity of 90.8%. Patients were stratified into low (0–1), moderate (2), and high (3) risk categories, which had NOM rates of 5.2%, 47.1%, and 77.8%, respectively.
Conclusions
Our prediction model may predict NOM failure in UA with good diagnostic accuracy and help surgeons select appropriate treatments.


Similar content being viewed by others
References
Fenyö G, Boijsen M, Enochsson L et al (2000) Acute abdomen calls for considerable care resources. Analysis of 3727 in-patients in the county of Stockholm during the first quarter of 1995 (article in Swedish). Lakartidningen 97:4008–4012
Laurell H, Hansson LE, Gunnarsson U (2013) Manifestations of acute appendicitis: a prospective study on acute abdominal pain. Dig Surg 30:198–206
Mällinen J, Vaarala S, Mäkinen M et al (2019) Appendicolith appendicitis is clinically complicated acute appendicitis–is it histopathologically different from uncomplicated acute appendicitis. Int J Colorectal Dis 34:1393–1400
Salminen P, Paajanen H, Rautio T et al (2015) Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA 313:2340–2348
Salminen P, Tuominen R, Paajanen H et al (2018) Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA 320:1259–1265
Podda M, Gerardi C, Cillara N et al (2019) Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic Review and meta-analysis. Ann Surg 270:1028–1040
Di Saverio S, Sibilio A, Giorgini E, Biscardi A et al (2014) The NOTA study (non operative treatment for acute appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg 260:109–117
Vons C, Barry C, Maitre S et al (2011) Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 377:1573–1579
van Dijk ST, van Dijk AH, Dijkgraaf MG et al (2018) Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis. Br J Surg 105:933–945
Alore EA, Ward JL, Todd SR et al (2018) Population-level outcomes of early versus delayed appendectomy for acute appendicitis using the American college of surgeons national surgical quality improvement program. J Surg Res 229:234–242
Shindoh J, Niwa H, Kawai K et al (2010) Predictive factors for negative outcomes in initial non-operative management of suspected appendicitis. J Gastrointest Surg 14:309–314
Loftus TJ, Brakenridge SC, Croft CA et al (2018) Successful nonoperative management of uncomplicated appendicitis: predictors and outcomes. J Surg Res 222:212-218.e2
Hong W, Kim MJ, Lee SM et al (2021) Computed tomography findings associated with treatment failure after antibiotic therapy for acute appendicitis. Korean J Radiol 22:63–71
Park HC, Kim MJ, Lee BH (2014) The outcome of antibiotic therapy for uncomplicated appendicitis with diameters ≤ 10 mm. Int J Surg 12:897–900
Wagner M, Tubre DJ, Asensio JA (2018) Evolution and current trends in the management of acute appendicitis. Surg Clin North Am 98:1005–1023
Andersson RE (2007) The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J Surg 31:86–92
Alaedeen DI, Cook M, Chwals WJ (2008) Appendiceal fecalith is associated with early perforation in pediatric patients. J Pediatr Surg 43:889–892
Almasaudi AS, McSorley ST, Horgan PG et al (2019) The relationship between body mass index, sex, and postoperative outcomes in patients undergoing potentially curative surgery for colorectal cancer. Clin Nutr ESPEN 30:185–189
Matsubara D, Arita T, Nakanishi M et al (2020) The impact of postoperative inflammation on recurrence in patients with colorectal cancer. Int J Clin Oncol 25:602–613
Almasaudi AS, McSorley ST, Edwards CA et al (2018) The relationship between body mass index and short term postoperative outcomes in patients undergoing potentially curative surgery for colorectal cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol 121:68–73
Balentine CJ, Wilks J, Robinson C et al (2010) Obesity increases wound complications in rectal cancer surgery. J Surg Res 163:35–39
Giefing-Kröll C, Berger P, Lepperdinger G et al (2015) How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell 14:309–321
Straub RH (2007) The complex role of estrogens in inflammation. Endocr Rev 28:521–574
Ashcroft GS, Greenwell-Wild T, Horan MA et al (1999) Topical estrogen accelerates cutaneous wound healing in aged humans associated with an altered inflammatory response. Am J Pathol 155:1137–1146
Kosyreva AM, Makarova OV, Kakturskiy LV et al (2018) Sex differences of inflammation in target organs, induced intraperitoneal injection of lipopolysaccharide, depend on its dose. J Inflamm Res 11:431–445
Hansson J, Khorram-Manesh A, Alwindawe A et al (2014) A model to select patients who may benefit from antibiotic therapy as the first line treatment of acute appendicitis at high probability. J Gastrointest Surg 18:961–967
Oliveira TM, de Faria FR, de Faria ER et al (2014) Nutritional status, metabolic changes and white blood cells in adolescents. Rev Paul Pediatr 32:351–359
Aminzadeh Z, Parsa E (2011) Relationship between Age and Peripheral White Blood Cell Count in Patients with Sepsis. Int J Prev Med 2:238–242
Acknowledgements
None.
Funding
No specific funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of informed consent
Informed consent was obtained from all individual participants included in the study.
Statement of human and animal rights
This study was approved by the Tokyo Medical University Hachioji Medical Center Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kobayashi, T., Hidaka, E., Koganezawa, I. et al. Prediction Model for Failure of Nonoperative Management of Uncomplicated Appendicitis in Adults. World J Surg 45, 3041–3047 (2021). https://doi.org/10.1007/s00268-021-06213-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06213-1