Abstract
Background
Tumours involving the supra-renal segment of IVC have dismal prognosis if left untreated. Currently, aggressive surgical management is the only potentially curative treatment but is associated with relatively high morbidity and mortality. This study aims to evaluate perioperative factors, associated with adverse postoperative outcomes, based on the perioperative characteristics and type of IVC reconstruction.
Methods
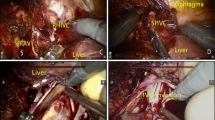
We identified 44 consecutive patients, who underwent supra-renal IVC resection with a mean age of 57.3 years. Isolated resection of IVC was performed in four patients, concomitant liver resection was performed in 27 patients and other associated resection in 13 patients. Total vascular exclusion was applied in 21 patients, isolated IVC occlusion in 11 patients. Neither venovenous bypass (VVB) nor hypothermic perfusion was used in any of the cases.
Results
The mean operative time was 205 min (150–324 min) and the mean estimated blood loss was 755 ml (230–4500 ml). Overall morbidity was 59% and major complications (Dindo-Clavien ≥ III) occurred in 11 patients (25%). The 90-day mortality was 11% (5pts). Intraoperative haemotransfusion was significantly associated with postoperative general complications (p < 0,001). With a mean follow-up of 26.2 months, the actuarial 1-, 3- and 5-year survival is 69%, 34%, and 16%, respectively.
Conclusions
IVC resection and reconstruction in the aspect of aggressive surgical management of malignant disease confers a survival advantage in patients, often considered unresectable. When performed in experienced centres it is associated with acceptable morbidity and mortality.




Similar content being viewed by others
References
Cady B (1983) Natural history of primary and secondary tumors of the liver. Semin Oncol 10(2):127–134
Rougier P, Milan C, Lazorthes F et al (1995) Prospective study of prognostic factors in patients with unresected hepatic metastases from colorectal cancer Fondation Francaise de Cancerologie Digestive. Br J Surg 82(10):1397–400
Mingoli A, Cavallaro A, Sapienza P et al (1996) International registry of inferior vena cava leiomyosarcoma: analysis of a world series on 218 patients. Anticancer Res 16(5b):3201–3205
Pringle JH (1908) Notes on the arrest of hepatic hemorrhage due to trauma. Ann Surg 48(4):541–9
Heaney JP, Stanton WK, Halbert DS et al (1966) An improved technic for vascular isolation of the liver: experimental study and case reports. Ann Surg 163(2):237–241
Huguet C, Nordlinger B, Galopin JJ et al (1978) Normothermic hepatic vascular exclusion for extensive hepatectomy. Surg Gynecol Obstet 147(5):689–693
Bismuth H, Castaing D, Garden OJ (1989) Major hepatic resection under total vascular exclusion. Ann Surg 210(1):13–19
Hannoun L, Panis Y, Balladur P et al (1991) Ex-situ in-vivo liver surgery. Lancet 337(8757):1616–1617
Miyazaki M, Ito H, Nakagawa K et al (1999) Aggressive surgical resection for hepatic metastases involving the inferior vena cava. Am J Surg 177(4):294–298
Madariaga JR, Fung J, Gutierrez J et al (2000) Liver resection combined with excision of vena cava. J Am Coll Surg 191(3):244–250
Okada Y, Nagino M, Kamiya J et al (2003) Diagnosis and treatment of inferior vena caval invasion by hepatic cancer. World J Surg 27(6):689–694
Arii S, Teramoto K, Kawamura T et al (2003) Significance of hepatic resection combined with inferior vena cava resection and its reconstruction with expanded polytetrafluoroethylene for treatment of liver tumors. J Am Coll Surg 196(2):243–249
Azoulay D, Andreani P, Maggi U et al (2006) Combined liver resection and reconstruction of the supra-renal vena cava: the Paul Brousse experience. Ann Surg 244(1):80–88
Malde DJ, Khan A, Prasad KR et al (2011) Inferior vena cava resection with hepatectomy: challenging but justified. HPB (Oxford) 13(11):802–810
Hemming AW, Mekeel KL, Zendejas I et al (2013) Resection of the liver and inferior vena cava for hepatic malignancy. J Am Coll Surg 217(1):115–24 (Discussion 124-5)
Nardo B, Ercolani G, Montalti R et al (2005) Hepatic resection for primary or secondary malignancies with involvement of the inferior vena cava: is this operation safe or hazardous? J Am Coll Surg 201(5):671–679
Bower TC, Nagorney DM, Cherry KJ Jr et al (2000) Replacement of the inferior vena cava for malignancy: an update. J Vasc Surg 31(2):270–281
Fiore M, Colombo C, Locati P et al (2012) Surgical technique, morbidity, and outcome of primary retroperitoneal sarcoma involving inferior vena cava. Ann Surg Oncol 19(2):511–518
Sweeney P, Wood CG, Pisters LL et al (2003) Surgical management of renal cell carcinoma associated with complex inferior vena caval thrombi. Urol Oncol 21(5):327–333
Navez J, Cauchy F, Dokmak S et al (2019) Complex liver resection under hepatic vascular exclusion and hypothermic perfusion with versus without veno-venous bypass: a comparative study. HPB (Oxford) 21(9):1131–1138
Azoulay D, Pascal G, Salloum C et al (2013) Vascular reconstruction combined with liver resection for malignant tumours. Br J Surg 100(13):1764–1775
Vladov NN, Mihaylov VI, Belev NV et al (2012) Resection and reconstruction of the inferior vena cava for neoplasms. World J Gastrointest Surg 4(4):96–101
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Vasilevski I, Takorov I, Mihaylov V et al (2019) Surgical outcomes and prognostic factors for survival for colorectal liver metastases: a 10-years single center experience. HPB 21:S800–S801
Isenberg J, Fischbach R, Kruger I et al (1996) Treatment of liver metastases from colorectal cancer. Anticancer Res 16(3a):1291–1295
Maeba T, Okano K, Mori S et al (2000) Extent of pathologic invasion of the inferior vena cava in resected liver cancer compared with possible caval invasion diagnosed by preoperative images. J Hepatobiliary Pancreat Surg 7(3):299–305
Hashimoto T, Minagawa M, Aoki T et al (2008) Caval invasion by liver tumor is limited. J Am Coll Surg 207(3):383–392
Eyraud D, Richard O, Borie DC et al (2002) Hemodynamic and hormonal responses to the sudden interruption of caval flow: insights from a prospective study of hepatic vascular exclusion during major liver resections. Anesth Analg 95(5):1173–8 (Table of contents)
Hannoun L, Delriviere L, Gibbs P et al (1996) Major extended hepatic resections in diseased livers using hypothermic protection: preliminary results from the first 12 patients treated with this new technique. J Am Coll Surg 183(6):597–605
Delva E, Barberousse JP, Nordlinger B et al (1984) Hemodynamic and biochemical monitoring during major liver resection with use of hepatic vascular exclusion. Surgery 95(3):309–318
Fortner JG, Shiu MH, Kinne DW et al (1974) Major hepatic resection using vascular isolation and hypothermic perfusion. Ann Surg 180(4):644–652
Azoulay D, Eshkenazy R, Andreani P et al (2005) In situ hypothermic perfusion of the liver versus standard total vascular exclusion for complex liver resection. Ann Surg 241(2):277–285
Hoffmann K, Weigand MA, Hillebrand N et al (2009) Is veno-venous bypass still needed during liver transplantation? A review of the literature. Clin Transplant 23(1):1–8
Budd JM, Isaac JL, Bennett J et al (2001) Morbidity and mortality associated with large-bore percutaneous venovenous bypass cannulation for 312 orthotopic liver transplantations. Liver Transpl 7(4):359–362
Azoulay D, Lim C, Salloum C et al (2015) Complex Liver Resection Using Standard Total Vascular Exclusion, Venovenous Bypass, and In Situ Hypothermic Portal Perfusion: An Audit of 77 Consecutive Cases. Ann Surg 262(1):93–104
Stattner S, Yip V, Jones RP et al (2014) Liver resection with concomitant inferior vena cava resection: experiences without veno-venous bypass. Surg Today 44(6):1063–1071
Torzilli G, Makuuchi M, Midorikawa Y et al (2001) Liver resection without total vascular exclusion: hazardous or beneficial? An analysis of our experience. Ann Surg 233(2):167–175
Oldhafer F, Ringe KI, Timrott K et al (2018) Modified ante situm liver resection without use of cold perfusion nor veno-venous bypass for treatment of hepatic lesions infiltrating the hepatocaval confluence. Langenbecks Arch Surg 403(3):379–386
Cauchy F, Brustia R, Perdigao F et al (2016) In Situ Hypothermic Perfusion of the Liver for Complex Hepatic Resection: Surgical Refinements. World J Surg 40(6):1448–1453
Machado MA, Herman P, Bacchella T et al (2007) Resection and reconstruction of retrohepatic vena cava without venous graft during major hepatectomies. J Surg Oncol 96(1):73–76
Miller CM, Schwartz ME, Nishizaki T (1991) Combined hepatic and vena caval resection with autogenous caval graft replacement. Arch Surg 126(1):106–108
Dale WA, Harris J, Terry RB (1984) Polytetrafluoroethylene reconstruction of the inferior vena cava. Surgery 95(5):625–630
Dokmak S, Aussilhou B, Sauvanet A et al (2015) Parietal Peritoneum as an Autologous Substitute for Venous Reconstruction in Hepatopancreatobiliary Surgery. Ann Surg 262(2):366–371
Pulitano C, Crawford M, Ho P et al (2013) Autogenous peritoneo-fascial graft: a versatile and inexpensive technique for repair of inferior vena cava. J Surg Oncol 107(8):871–872
Hobeika C, Cauchy F, Soubrane O (2020) Case series of extended liver resection associated with inferior vena cava reconstruction using peritoneal patch. Int J Surg 80:6–11
Addeo P, Rosso E, Oussoultzoglou E et al (2012) Inferior vena cava graft-enteric fistula after extended hepatectomy with caval replacement. J Vasc Surg 55(1):226–229
Gloviczki P, Hollier LH, Dewanjee MK et al (1984) Experimental replacement of the inferior vena cava: factors affecting patency. Surgery 95(6):657–666
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Nikola Vladov was involved in study concept and design; Maria Yakova, Tsvetan Trichkov contributed to acquisition of data ; Radoslav Kostadinov, Vassil Mihaylov, Evelina Odisseeva were involved in analysis and interpretation of data; Radoslav Kostadinov, Ivelin Takorov contributed to drafting of manuscript; Tsonka Lukanova, Ventsislav Mutafchiyski, Nikola Vladov were involved in critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was waived by the local Ethics Committee of Military Medical Academy—Sofia given the retrospective nature of the study and all the procedures being performed were part of the routine care.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vladov, N., Kostadinov, R., Mihaylov, V. et al. Single-Centre Experience of Supra-Renal Vena Cava Resection and Reconstruction. World J Surg 45, 2270–2279 (2021). https://doi.org/10.1007/s00268-021-06048-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06048-w