Abstract
Introduction
The relationship between hospital volume and outcomes remains unclear in the delivery of burn care in resource-limited settings, where demand often exceeds capacity. We sought to characterize the association between burn patient volume and the use of operative intervention at a tertiary burn unit in Malawi.
Methods
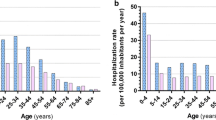
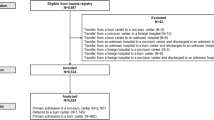
This study examined patients admitted to Kamuzu Central Hospital located in Lilongwe, Malawi, over years 2011–2019. We described the association between the census at the time of admission and the use of operative intervention, as well as the time to operation. Patient census was defined as low (≤ 15 patients), medium (16–29 patients), and high (≥ 30 patients).
Results
A total of 2484 patients were included. The mean daily burn unit census was 22.5 patients (SD 6.6) and varied significantly by season. For the medium and high census, the adjusted risk ratio of undergoing surgery was 0.79 (95% CI 0.64, 0.97) and 0.65 (95% CI 0.49, 0.85), respectively, adjusted for flame burn, age, %TBSA, and delayed presentation. At a low admission census, the adjusted mean time to operation was 17.2 days (95% CI 14.4, 20.1) compared to 28.3 days (95% CI 25.4, 31.2) at a high census.
Conclusions
In a resource-limited setting, an increasing mean daily census significantly reduced the use of operative intervention and increased time to operation, potentially increasing burn-associated morbidity. In order to improve the quality of burn care in similar environments, improved resource allocation during busier seasons and targeted burn prevention efforts are imperative.


Similar content being viewed by others
References
Peck MD (2011) Epidemiology of burns throughout the world. Part I: distribution and risk factors. Burns 37:1087–1100
Nthumba PM (2016) Burns in sub-Saharan Africa: a review. Burns 42:258–266
Meara JG, Leather AJ, Hagander L et al (2015) Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386:569–624
Papini R (2004) Management of burn injuries of various depths. BMJ 329:158–160
Sheridan RL, Tompkins RG, Burke JF (1994) Management of burn wounds with prompt excision and immediate closure. J Intensive Care Med 9:6–19
Kiser M, Beijer G, Mjuweni S et al (2013) Photographic assessment of burn wounds: a simple strategy in a resource-poor setting. Burns 39:155–161
Zou G (2004) A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706
Chen W, Qian L, Shi J et al (2018) Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol 18:63
Maine R, Kajombo C, Purcell L et al (2019) Effect of in-hospital delays on surgical mortality for emergency general surgery conditions at a tertiary hospital in Malawi. BJS open 3:367
Kong VY, Van de Linde S, Aldous C et al (2013) Quantifying the disparity in outcome between urban and rural patients with acute appendicitis in South Africa. S Afr Med J 103:742–745
Purcell LN, Robinson B, Msosa V et al (2020) District general hospital surgical capacity and mortality trends in patients with Acute Abdomen in Malawi. World J Surg 12:1–8https://doi.org/10.1007/s00268-020-05468-4
Ong YS, Samuel M, Song C (2006) Meta-analysis of early excision of burns. Burns 32:145–150
Charles AG, Gallaher J, Cairns BA (2017) Burn care in low- and middle-income Countries. Clin Plast Surg 44:479–483
Gallaher JR, Banda W, Robinson B et al (2020) Access to operative intervention reduces mortality in adult burn patients in a resource-limited setting in Sub-Saharan Africa. World J Surg 44:3629–3635. https://doi.org/10.1007/s00268-020-05684-y
Purcell LN, Banda W, Williams B et al (2020) The effect of surgical intervention on pediatric burn injury survival in a resource-poor setting. J Surg Res 253:86–91
Hsia RY, Mbembati NA, Macfarlane S et al (2012) Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy Plan 27:234–244
Tyson AF, Gallaher J, Mjuweni S et al (2017) The effect of seasonality on burn incidence, severity and outcome in Central Malawi. Burns 43:1078–1082
Chelidze KI, Lim CC, Peck RN et al (2016) Predictors of mortality among pediatric burn patients in East Africa. J Burn Care Res 37:e154–e160
Gallaher JR, Mjuweni S, Shah M et al (2015) Timing of early excision and grafting following burn in sub-Saharan Africa. Burns 41:1353–1359
Tyson AF, Boschini LP, Kiser MM et al (2013) Survival after burn in a sub-Saharan burn unit: challenges and opportunities. Burns 39:1619–1625
Charles JM, Jones A, Lloyd-Williams H (2019) Return on investment, social return on investment, and the business case for prevention. Appl Health Econ Public Health Pract Res. https://doi.org/10.1093/med/9780198737483.003.0012
Rybarczyk MM, Schafer JM, Elm CM et al (2016) Prevention of burn injuries in low-and middle-income countries: a systematic review. Burns 42:1183–1192
Mock C PM, Peden M, Krug E, eds (2008) A WHO plan for burn prevention and care. Bulletin of the World Health Organization. 2009;87:802-3
Acknowledgements
Study data were collected and managed using REDCap electronic data capture tools hosted at UNC. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing: (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for importing data from external sources.
Funding
The Department of Surgery at the University of North Carolina provided funding for this study.
Author information
Authors and Affiliations
Contributions
JG contributed to study design, data acquisition, analysis, and drafting of manuscript. LP contributed to acquisition of data, analysis, and drafting of manuscript. WB contributed to study design, acquisition of data, and critical revisions of manuscript. TR contributed to study design, acquisition of data, analysis, and critical revision of manuscript. AC contributed to study design, analysis, drafting of manuscript, and project supervision.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gallaher, J., Purcell, L.N., Banda, W. et al. The Association Between Burn Unit Census and Operative Intervention in a Resource-Limited Setting. World J Surg 45, 1686–1691 (2021). https://doi.org/10.1007/s00268-021-06037-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06037-z