Abstract
Background
The majority of patients with non-metastatic breast cancer will undergo surgery. This involves complex decisions that inevitably increase time from diagnosis to surgery beyond the currently recommended 30 days. This study aims to analyse factors that increase time to surgery and establish whether it is justifiable in the context of improved individualised breast cancer management.
Methods
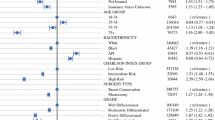
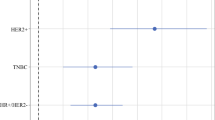
A retrospective analysis of all patients at Austin Health surgically managed for non-metastatic invasive breast carcinoma between 2013 and 2019 was conducted. Time to surgery (TTS) was defined as time between informed diagnosis and cancer surgery. The patients were grouped into TTS groups of ≤30 days and >30 days. Kaplan–Meier survival analysis and Cox proportional hazards regression model were used to evaluate the impact of time interval between diagnosis and surgery.
Results
Seven hundred and thirty-one patients were included in our TTS analysis, only half of this cohort received surgery within the recommended 30 days. Many of the factors identified to be associated with increased TTS are the key to optimal management. Median follow-up for the cohort was 30 months. Between wait groups of ≤30 and >30 days, there were no significant association found between TTS and survival outcomes for DFS (HR 1.20 95% CI 0.56–2.60) and OS (HR 1.58 95% CI 0.82–3.03).
Conclusion
Breast cancer management involves complex factors that significantly increase TTS. Surgery within 30 days of diagnosis is not associated with improved DFS and OS. Outcomes from this study support a revision of current recommendations for TTS in non-metastatic breast cancer care.


Similar content being viewed by others
Abbreviations
- BCS:
-
Breast conserving surgery
- CT:
-
Computer tomography
- DFS:
-
Disease-free survival
- ER:
-
Oestrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hazard ratio
- MRI:
-
Magnetic resonance imaging
- NCDB:
-
National Cancer Database
- OS:
-
Overall survival
- PR:
-
Rogesterone receptor
- SEER-Medicare:
-
Surveillance, Epidemiology and End Results-Medicare
References
Breast Cancer Statistics American Institute for Cancer Research 2019 [cited 2019 1st April]. https://www.wcrf.org/dietandcancer/cancer-trends/breast-cancer-statistics
Breast Cancer Statistics in Australia Australian Government Cancer Australia 2019 [cited 2019 1st April]. https://breast-cancer.canceraustralia.gov.au/statistics
Smith DB, Jiang J, McLaughlin SS et al (2011) Improvement in breast cancer outcomes over time: are older women missing out? J Clin Oncol 29(35):4647–4653
Bardell T, Belliveau P, Kong W et al (2006) Waiting times for cancer surgery in Ontario: 1984–2000. Clin Oncol 18(5):401–409
Bilimoria KY, Ko CY, Tomlinson JS et al (2011) Wait times for cancer surgery in the United States. Ann Surg 253(4):779–785
Hulvat M, Sandalow N, Rademaker A et al (2010) Time from diagnosis to definitive operative treatment of operable breast cancer in the era of multimodal imaging. Surgery 148(4):746–750 discussion 50–51
Bleicher RJ, Ruth K, Sigurdson ER et al (2012) Preoperative delays in the US Medicare population with breast cancer. J Clin Oncol 30(36):4485–4492
Liederbach E, Sisco M, Wang C et al (2015) Wait times for breast surgical operations, 2003–2011: a report from the National Cancer Data Base. Ann Surg Oncol 22(3):899–907
Sainsbury JR, Johnston C, Haward B (1999) Effect on survival of delays in referral of patients with breast-cancer symptoms: a retrospective analysis. The Lancet 353(9159):1132–1135
Rosselli Del Turco M, Ponti A, Bick U, Biganzoli L et al (2010) Quality indicators in breast cancer care. Eur J Cancer 46(13):2344–2356
Fallowfield LJ, Hall A, Maguire P et al (1994) Psychological effects of being offered choice of surgery for breast cancer. BMJ 309:448
Bleicher RJ, Ciocca RM, Egleston BL et al (2009) Association of routine pretreatment magnetic resonance imaging with time to surgery, mastectomy rate, and margin status. J Am Coll Surg 209(2):180–187
Bleicher RJ (2018) Timing and delays in breast cancer evaluation and treatment. Ann Surg Oncol 25(10):2829–2838
Brazda A, Estroff J, Euhus D et al (2010) Delays in time to treatment and survival impact in breast cancer. Ann Surg Oncol 17(Suppl 3):291–296
Richards MA, Westcombe AM, Love SB et al (1999) Influence of delay on survival in patients with breast cancer: a systematic review. The Lancet 353(9159):1119–1126
Yoo T-K, Han W, Moon H-G et al (2016) Delay of treatment initiation does not adversely affect survival outcome in breast cancer. Cancer Research and Treatment 48(3):962–969
Eriksson L, Bergh J, Humphreys K et al (2018) Time from breast cancer diagnosis to therapeutic surgery and breast cancer prognosis: a population-based cohort study. Int J Cancer 143(5):1093–1104
Mansfield SA, Abdel-Rasoul M, Terando AM et al (2017) Timing of breast cancer surgery—how much does it matter? Breast J 23(4):444–451
McLaughlin JM, Anderson RT, Ferketich AK et al (2012) Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. J Clin Oncol 30(36):4493–4500
Mujar M, Dahlui M, Yip CH et al (2013) Delays in time to primary treatment after a diagnosis of breast cancer: does it impact survival? Prev Med 56(3–4):222–224
Shin DW, Cho J, Kim SY et al (2013) Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol 20(8):2468–2476
Smith EC, Ziogas A, Anton-Culver H (2013) Delay in surgical treatment and survival after breast cancer diagnosis in young women by race/ethnicity. JAMA Surg 148(6):516–523
Royal Australasian College of Surgeons (2015) National elective surgery urgency categorisation.
Vujovic O, Yu E, Cherian A et al (2009) Effect of interval to definitive breast surgery on clinical presentation and survival in early-stage invasive breast cancer. Int J Radiat Oncol Biol Phys 75(3):771–774
Bleicher RJ, Ruth K, Sigurdson ER et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Wagner JL, Warneke CL, Mittendorf EA et al (2011) Delays in primary surgical treatment are not associated with significant tumor size progression in breast cancer patients. Ann Surg 254(1):119–124
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research project did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. The authors declare that they have no conflict of interest.
Ethical approval
This project received ethical approval from the Austin Health Human Research Ethics Committee (HREC) 17 August 2018. The HREC confirms that the project meets the requirements of the National Statement on Ethical Conduct in Human Research (2007).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, J., Bromley, L., Chew, G. et al. “First Do No Harm”: Significance of Delays from Diagnosis to Surgery in Patients with Non-metastatic Breast Cancer. World J Surg 44, 3812–3820 (2020). https://doi.org/10.1007/s00268-020-05725-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05725-6