Abstract
Background
To identify risk factors of postoperative cranial nerve injury (CNI) following surgical treatment of a carotid body tumor (CBT) by retrospective analysis of the data during the past decade in our center.
Methods
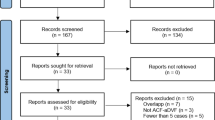
From May 2008 to September 2018, patients who underwent CBT resections at the Department of Vascular Surgery, Zhongshan Hospital, Fudan University, were included in the study. Demographic, preoperative, intraoperative, and postoperative data of patients were collected and analyzed. Univariate and multivariate logistic regression analyses were performed to identify the independent risk factors of CNI.
Results
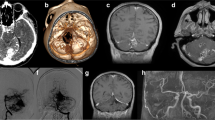
A total of 203 CBTs were excised in 196 patients; 17.7% was classified as Shamblin I, 59.1% as Shamblin II, and 23.2% as Shamblin III. CNI after surgery occurred in 57 (28.1%) patients. Postoperative CNI, external carotid artery (ECA) ligation, internal carotid artery (ICA) reconstruction, tumor volume, and established blood loss (EBL) were significantly correlated with Shamblin classification. On univariate analysis, there were statistically significant differences in Shamblin classification (p = 0.002), tumor volume (p = 0.014), number of lymph nodes removed (NOLNR) (p < 0.001), and EBL (p = 0.019) between two groups (with and without CNI after surgery). Multivariate logistic regression analysis revealed a significant positive correlation between CNI and Shamblin III (AOR, 4.744; 95% CI, 1.21–18.56; p = 0.025) and NOLNR (AOR, 0.25; 95% CI, 1.23–1.46 for each three-interval increase, p < 0.001).
Conclusions
Shamblin III and NOLNR are independent risk factors of CNI for patients who undergo CBT resections.
Similar content being viewed by others
References
Boedeker CC, Ridder GJ, Schipper J (2005) Paragangliomas of the head and neck: diagnosis and treatment. Fam Cancer 4:55–59
Hallett JW Jr, Nora JD, Hollier LH et al (1988) Trends in neurovascular complications of surgical management for carotid body and cervical paragangliomas: a fifty-year experience with 153 tumors. J Vasc Surg 7:284–291
Metheetrairut C, Chotikavanich C, Keskool P et al (2016) Carotid body tumor: a 25-year experience. Eur Arch Otorhinolaryngol 273:2171–2179
Davila VJ, Chang JM, Stone WM et al (2016) Current surgical management of carotid body tumors. J Vasc Surg 64:1703–1710
Straughan DM, Neychev VK, Sadowski SM et al (2015) Preoperative imaging features are associated with surgical complications following carotid body tumor resection. World J Surg 39:2084–2089. https://doi.org/10.1007/s00268-015-3058-9
Kim GY, Lawrence PF, Moridzadeh RS et al (2017) New predictors of complications in carotid body tumor resection. J Vasc Surg 65:1673–1679
Shamblin WR, ReMine WH, Sheps SG et al (1971) Carotid body tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am J Surg 122:732–739
Kruger AJ, Walker PJ, Foster WJ et al (2010) Important observations made managing carotid body tumors during a 25-year experience. J Vasc Surg 52:1518–1523
Casarim AL, Tincani AJ, Del Negro A et al (2014) Carotid body tumor: retrospective analysis on 22 patients. Sao Paulo Med J 132:133–139
Dionigi G, Bacuzzi A, Boni L et al (2008) What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg 6(Suppl 1):S7–12
Wong KP, Mak KL, Wong CK et al (2017) Systematic review and meta-analysis on intraoperative neuromonitoring in high-risk thyroidectomy. Int J Surg 38:21–30
Hei H, Zhou B, Qin J et al (2016) Intermittent intraoperative nerve monitoring in thyroid reoperations: Preliminary results of a randomized, single-surgeon study. Head Neck 38(Suppl l):E1993–E1997
Yang SW, Zhou L, Lu Z et al (2017) Systematic review with meta-analysis of intraoperative neuromonitoring during thyroidectomy. Int J Surg 39:104–113
Srajcich BC, McHenry CR (2016) The utility of intraoperative nerve monitoring during thyroid surgery. J Surg Res 204:29–33
Amato B, Bianco T, Compagna R et al (2014) Surgical resection of carotid body paragangliomas: 10 years of experience. Am J Surg 207:293–298
Law Y, Chan YC, Cheng SW (2017) Surgical management of carotid body tumor - Is Shamblin classification sufficient to predict surgical outcome? Vascular 25:184–189
Cunningham EJ, Bond R, Mayberg MR et al (2004) Risk of persistent cranial nerve injury after carotid endarterectomy. J Neurosurg 101:445–448
Kim GY, Lawrence PF, Munoz A et al (2015) Predictors of neurovascular complications in carotid body tumor resection. J Vasc Surg 61:146S–147S
Bennett KM, Scarborough JE, Shortell CK (2015) Risk factors for cranial nerve injury after carotid endarterectomy. J Vasc Surg 62:363–368
Kasper GC, Welling RE, Wladis AR et al (2006) A multidisciplinary approach to carotid paragangliomas. Vasc Endovascular Surg 40:467–474
Anand VK, Alemar GO, Sanders TS (1995) Management of the internal carotid artery during carotid body tumor surgery. Laryngoscope 105:231–235
Nunez DA, Lang W, Pollock JG (1989) Associated carotid body tumour and pharyngeal pouch. J Laryngol Otol 103:531–532
Lee JH, Barich F, Karnell LH et al (2002) National cancer data base report on malignant paragangliomas of the head and neck. Cancer 94:730–737
Martin CE, Rosenfeld L, McSwain B (1973) Carotid body tumors: a 16-year follow-up of seven malignant cases. South Med J 66:1236–1243
Pacheco-Ojeda LA (2017) Carotid body tumors: Surgical experience in 215 cases. J Craniomaxillofac Surg 45:1472–1477
Acknowledgements
Grant support: This work was supported by the training program for outstanding academic leaders of the Shanghai health and family planning system [Hundred Talent Program, grant number 2018BR40]; China National Natural Science Funds [Grant No. 30801122]; and Shanghai Rising-Star Program [grant number 19XD1401200].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Informed consent
Obtained from all individual participants included in the study.
This study design was approved by the Ethics Committee of Zhongshan Hospital, Fudan University, Shanghai, China.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiang, X., Fang, G., Guo, D. et al. Surgical Management of Carotid Body Tumor and Risk Factors of Postoperative Cranial Nerve Injury. World J Surg 44, 4254–4260 (2020). https://doi.org/10.1007/s00268-020-05723-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05723-8