Abstract
Background
Population-based analyses of 30-day outcomes after parathyroidectomy for renal secondary hyperparathyroidism are limited. We sought to identify risk factors associated with prolonged length of stay (LOS) and readmission in this patient population.
Methods
Patients with secondary hyperparathyroidism who underwent parathyroidectomy were reviewed in the ACS-NSQIP database (2011–2016). Patients were identified by ICD codes specific to secondary hyperparathyroidism of renal origin and the ACS-NSQIP variable for current preoperative dialysis. Multivariable logistic regression was used to identify independent factors associated with prolonged LOS and 30-day readmission after parathyroidectomy.
Results
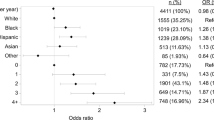
The cohort included 1846 patients with secondary hyperparathyroidism on dialysis who underwent parathyroidectomy. There were 416 (22.5%) patients classified under the prolonged LOS group. On multivariable analysis, factors associated with prolonged LOS included elevated preoperative alkaline phosphatase [OR 3.13 (95%-CI 2.09–4.70), p < 0.001], decreased preoperative hematocrit [OR 1.83 (95%-CI 1.25–2.68), p = 0.002], unplanned reoperation (OR 5.02 [95%-CI 2.22–11.3], p < 0.001) and any postoperative complication [OR 6.12 (95%-CI 3.31–11.3), p < 0.001]. The overall 30-day readmission rate was 15.0%. Hypocalcemia and hungry bone syndrome accounted for 47.0% (n = 93/198) of readmissions. On multivariable analysis, patients with a history of hypertension and those undergoing unplanned reoperation were at risk of readmission [2.16 (95%-CI 1.21–3.87), p = 0.009, and 2.40 (95%-CI 1.15–5.02), p = 0.020, respectively], whereas reoperative parathyroidectomy was inversely associated with readmission (OR 0.24, 95%-CI 0.07–0.80, p = 0.021).
Conclusion
In patients undergoing parathyroidectomy for renal secondary hyperparathyroidism, several readily available preoperative biochemical markers, including those of increased bone turnover and anemia, are associated with prolonged postoperative LOS. Unplanned reoperation was predictive of both increased LOS and readmission.


Similar content being viewed by others
References
Sitges-Serra A, Caralps-Riera A (1987) Hyperparathyroidism associated with renal disease. Pathogenesis, natural history, and surgical treatment. Surg Clin North Am 67:359–377
Tentori F, Wang M, Bieber BA et al (2015) Recent changes in therapeutic approaches and association with outcomes among patients with secondary hyperparathyroidism on chronic hemodialysis: the DOPPS study. Clin J Am Soc Nephrol 10:98–109. https://doi.org/10.2215/CJN.12941213
Levin A, Bakris GL, Molitch M et al (2007) Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int 71:31–38. https://doi.org/10.1038/sj.ki.5002009
Saliba W, El-Haddad B (2009) Secondary hyperparathyroidism: pathophysiology and treatment. J Am Board Fam Med 22:574–581. https://doi.org/10.3122/jabfm.2009.05.090026
Cozzolino M, Gallieni M, Corsi C et al (2004) Management of calcium refilling post-parathyroidectomy in end-stage renal disease. J Nephrol 17:3–8
Ho L-Y, Wong P-N, Sin H-K et al (2017) Risk factors and clinical course of hungry bone syndrome after total parathyroidectomy in dialysis patients with secondary hyperparathyroidism. BMC Nephrol 18:12. https://doi.org/10.1186/s12882-016-0421-5
Torer N, Torun D, Torer N et al (2009) Predictors of early postoperative hypocalcemia in hemodialysis patients with secondary hyperparathyroidism. Transpl Proc 41:3642–3646. https://doi.org/10.1016/j.transproceed.2009.06.207
Shoback D (2008) Clinical practice. Hypoparathyroidism. N Engl J Med 359:391–403. https://doi.org/10.1056/NEJMcp0803050
Lau WL, Obi Y, Kalantar-Zadeh K (2018) Parathyroidectomy in the management of secondary hyperparathyroidism. Clin J Am Soc Nephrol 13:952–961. https://doi.org/10.2215/CJN.10390917
Jain N, Reilly RF (2017) Hungry bone syndrome. Curr Opin Nephrol Hypertens 26:250–255. https://doi.org/10.1097/MNH.0000000000000327
Yajima A, Ogawa Y, Takahashi HE et al (2003) Changes of bone remodeling immediately after parathyroidectomy for secondary hyperparathyroidism. Am J Kidney Dis 42:729–738
Cruz DN, Perazella MA (1997) Biochemical aberrations in a dialysis patient following parathyroidectomy. Am J Kidney Dis 29:759–762
Brasier AR, Nussbaum SR (1988) Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med 84:654–660. https://doi.org/10.1016/0002-9343(88)90100-3
Witteveen JE, van Thiel S, Romijn JA, Hamdy NAT (2013) Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol 168:R45–53. https://doi.org/10.1530/EJE-12-0528
Viaene L, Evenepoel P, Bammens B et al (2008) Calcium requirements after parathyroidectomy in patients with refractory secondary hyperparathyroidism. Nephron Clin Pract 110:c80–c85. https://doi.org/10.1159/000151722
Mittendorf EA, Merlino JI, McHenry CR (2004) Post-parathyroidectomy hypocalcemia: incidence, risk factors, and management. Am Surg 70:114–119 Discussion 119
Ferrandino R, Roof S, Ma Y et al (2017) Unplanned 30-day readmissions after parathyroidectomy in patients with chronic kidney disease: a nationwide analysis. Otolaryngol Head Neck Surg 157:955–965. https://doi.org/10.1177/0194599817721154
Jofré R, López Gómez JM, Menárguez J et al (2003) Parathyroidectomy: Whom and When? Kidney Int Suppl. https://doi.org/10.1046/j.1523-1755.63.s85.23.x
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Shiloach M, Frencher SK, Steeger JE et al (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210:6–16. https://doi.org/10.1016/j.jamcollsurg.2009.09.031
Raval MV, Pawlik TM (2018) Practical guide to surgical data sets: national surgical quality improvement program (NSQIP) and pediatric NSQIP. JAMA Surg 153:764–765. https://doi.org/10.1001/jamasurg.2018.0486
American College of Surgeons National Surgical Quality Improvement Program (2020) Data collection, analysis and reporting. Chicago, IL. Available from http://site.acsnsqip.org/program-specifics/data-collection-analysis-and-reporting/
Xia H, Ebben J, Ma JZ, Collins AJ (1999) Hematocrit levels and hospitalization risks in hemodialysis patients. J Am Soc Nephrol 10:1309–1316
Hu W-H, Cajas-Monson LC, Eisenstein S et al (2015) Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 14:91. https://doi.org/10.1186/s12937-015-0081-5
Cheng S-P, Liu C-L, Chen H-H et al (2009) Prolonged hospital stay after parathyroidectomy for secondary hyperparathyroidism. World J Surg 33:72–79. https://doi.org/10.1007/s00268-008-9787-2
Niramitmahapanya S, Sunthornthepvarakul T, Deerochanawong C et al (2011) Role of loading calcitriol to control hypocalcemia after parathyroidectomy in chronic kidney disease. J Med Assoc Thai 94:295–302
Alsafran S, Sherman SK, Dahdaleh FS et al (2019) Preoperative calcitriol reduces postoperative intravenous calcium requirements and length of stay in parathyroidectomy for renal-origin hyperparathyroidism. Surgery 165:151–157. https://doi.org/10.1016/j.surg.2018.03.029
Latus J, Roesel M, Fritz P et al (2013) Incidence of and risk factors for hungry bone syndrome in 84 patients with secondary hyperparathyroidism. Int J Nephrol Renovasc Dis 6:131–137. https://doi.org/10.2147/IJNRD.S47179
Portolés J, López-Gómez JM, Aljama P (2007) A prospective multicentre study of the role of anaemia as a risk factor in haemodialysis patients: the MAR Study. Nephrol Dial Transpl 22:500–507. https://doi.org/10.1093/ndt/gfl558
Zhang Y, Thamer M, Stefanik K et al (2004) Epoetin requirements predict mortality in hemodialysis patients. Am J Kidney Dis 44:866–876
Locatelli F, Pisoni RL, Akizawa T et al (2004) Anemia management for hemodialysis patients: kidney disease outcomes quality initiative (K/DOQI) guidelines and dialysis outcomes and practice patterns study (DOPPS) findings. Am J Kidney Dis 44:27–33. https://doi.org/10.1053/j.ajkd.2004.08.008
Dakour-Aridi H, Nejim B, Locham S et al (2019) Anemia and postoperative outcomes after open and endovascular repair of intact abdominal aortic aneurysms. J Vasc Surg 69:738–751.e2. https://doi.org/10.1016/j.jvs.2018.05.233
Phan K, Wang N, Kim JS et al (2017) Effect of preoperative anemia on the outcomes of anterior cervical discectomy and fusion. Glob Spine J 7:441–447. https://doi.org/10.1177/2192568217699404
Venkat R, Guerrero MA (2015) Risk factors and outcomes of blood transfusions in adrenalectomy. J Surg Res 199:505–511. https://doi.org/10.1016/j.jss.2015.06.042
Blaudszun G, Munting KE, Butchart A et al (2018) The association between borderline pre-operative anaemia in women and outcomes after cardiac surgery: a cohort study. Anaesthesia 73:572–578. https://doi.org/10.1111/anae.14185
Murji A, Lam M, Allen B et al (2019) Risks of pre-operative anemia in women undergoing elective hysterectomy and myomectomy. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2019.07.018
Michailidou M, Nfonsam VN (2018) Preoperative anemia and outcomes in patients undergoing surgery for inflammatory bowel disease. Am J Surg 215:78–81. https://doi.org/10.1016/j.amjsurg.2017.02.016
Roche AM, Brant JA, Chai RL (2018) Predictors of readmission and reoperation in patients undergoing parathyroidectomy for primary hyperparathyroidism. Otolaryngol Head Neck Surg 158:828–834. https://doi.org/10.1177/0194599818758019
Kuo LE, Wachtel H, Karakousis G et al (2014) Parathyroidectomy in dialysis patients. J Surg Res 190:554–558. https://doi.org/10.1016/j.jss.2014.05.027
Kuo LE, Wachtel H, Fraker D, Kelz R (2014) Reoperative parathyroidectomy: Who is at risk and What is the risk? J Surg Res 191:256–261. https://doi.org/10.1016/j.jss.2014.05.073
Margolick J, Wiseman SM (2018) Risk of major complications following thyroidectomy and parathyroidectomy: Utility of the NSQIP surgical risk calculator. Am J Surg 215:936–941. https://doi.org/10.1016/j.amjsurg.2018.01.006
Guillén Martínez AJ, Smilg Nicolás C, Moraleda Deleito J et al (2019) Risk factors and evolution of calcium and parathyroid hormone levels in hungry bone syndrome after parthyroidectomy for primary hyperparathyroidism. Endocrinol Diabetes Nutr. https://doi.org/10.1016/j.endinu.2019.05.011
Yang M, Zhang L, Huang L et al (2016) Factors predictive of critical value of hypocalcemia after total parathyroidectomy without autotransplantation in patients with secondary hyperparathyroidism. Ren Fail 38:1224–1227. https://doi.org/10.1080/0886022X.2016.1202731
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no disclosures or financial support for this work.
Human and animal rights
The study was approved by the institutional review board at Weill Cornell Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stefanova, D., Ullmann, T.M., Limberg, J. et al. Risk Factors for Prolonged Length of Stay and Readmission After Parathyroidectomy for Renal Secondary Hyperparathyroidism. World J Surg 44, 3751–3760 (2020). https://doi.org/10.1007/s00268-020-05711-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05711-y