Abstract
Background
The present study compared the short-term outcomes and costs of laparoscopic distal gastrectomy (LDG) with those of open distal gastrectomy (ODG) for gastric cancer using a nationwide administrative database in Japan.
Method
Overall, 37,752 patients with gastric cancer who underwent distal gastrectomy at 1074 hospitals in the fiscal year 2012–2013 were evaluated using a diagnosis procedure combination database in Japan. We performed a retrospective analysis via a multilevel analysis (MLA) of the short-term surgical results and costs of the LDG and ODG groups. The models included the age, sex, comorbid complications, smoking, body mass index (BMI), activity of daily living (ADL), stage, and the number of cases of gastrectomy per facility for adjustment. The in-hospital mortality relative to the hospital volume was also compared.
Results
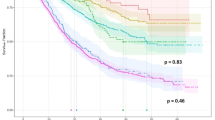
The LDG group required postoperative blood transfusion less frequently and had fewer postoperative complications, shorter hospitalization, and lower operative mortality than the ODG group. While this stage did not correlate with the in-hospital mortality, the surgical method, age, sex, ADL, BMI, comorbidity, and yearly volume showed a correlation. A significant association in the in-hospital mortality was observed between low- and very-high-volume hospitals.
Conclusion
In this large nationwide cohort of patients with gastric cancer using an MLA, LDG was shown to be safer with lower mortality and postoperative complication rates than ODG.

Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
https://ganjoho.jp/reg_stat/statistics/stat/summary.html, from the website of Cancer information service, National Cancer Center
Katai H, Sasako M, Fukuda H et al (2010) JCOG gastric cancer surgical study. Safety and feasibility of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG 0703). Gastric Cancer 13:238–244
Kim HH, Hyung WJ, Cho GS et al (2010) Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report—a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg 251:417–420
Takiguchi S, Fujiwara Y, Yamasaki M et al (2013) Laparoscopy-assisted distal gastrectomy versus open distal gastrectomy. A prospective randomized single-blind study. World J Surg 37:2379–2386. https://doi.org/10.1007/s00268-013-2121-7
Kitano S, Shiraishi N, Fujii K et al (2002) A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery 131:S306–S311
Sakuramoto S, Yamashita K, Kikuchi S et al (2013) Laparoscopy versus open distal gastrectomy by expert surgeons for early gastric cancer in Japanese patients: short-term clinical outcomes of a randomized clinical trial. Surg Endosc 27:1695–1705
Kuwabara K, Matsuda S, Fushimi K et al (2011) Quantitative assessment of the advantages of laparoscopic gastrectomy and the impact of volume-related hospital characteristics on resource use and outcomes of gastrectomy patients in Japan. Ann Surg 253:64–70
Yasunaga H, Horiguchi H, Kuwabara K et al (2013) Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann Surg 257:640–646
Birkmeyer JD, Siewers AE, Finlayson EV et al (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346:1128–1137
Begg CB, Cramer LD, Hoskins WJ et al (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280:1747–1751
Dudley RA, Johansen KL, Brand R et al (2000) Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA 283:1159–1166
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137:511–520
Killeen SD, O’Sullivan MJ, Coffey JC et al (2005) Provider volume and outcomes for oncological procedures. Br J Surg 392:389–402
Suzuki H, Gotoh M, Sugihara K et al (2011) Nationwide survey and establishment of a clinical database for gastrointestinal surgery in Japan: targeting integration of a cancer registration system and improving the outcome of cancer treatment. Cancer Sci 102:226–230
Goldstein H. Multilevel statistical models. 3. London: Arnold; 2003
Kreft I, Leeuw JD (1998) Introducing multilevel modeling. Sage, London
Twisk JWR (2006) Applied multilevel analysis: a practical guide. Cambridge University Press, Cambridge
Goldstein H (2003) Multilevel statistical models. Bedford Group for Life Course and Statistical Studies, London
Anglemyer A, Horvath HT, Bero L (2014) Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev 4:MR000034
Zhang Z, Ni H, Xu X (2014) Observational studies using propensity score analysis underestimated the effect sizes in critical care medicine. J Clin Epidemiol 67:932–939
Dahabreh IJ, Sheldrick RC, Paulus JK et al (2012) Do observational studies using propensity score methods agree with randomized trials? A systematic comparison of studies on acute coronary syndromes. Eur Heart J 33:1893–1901
Rousenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Rubin D (1997) Estimating causal effects from large data sets using propensity scores. Ann Intern Med 127:757–773
Iwatsuki M, Yamamoto H, Miyata H et al (2019) Effect of hospital and surgeon volume on postoperative outcomes after distal gastrectomy for gastriccancer based on data from 145,523 Japanese patients collected from a nationwide web-based data entry system. Gastric Cancer 22:190–201
Wainess RM, Dimick JB, Upchurch GR Jr et al (2003) Epidemiology of surgically treated gastric cancer in the United States, 1988–2000. J Gastrointest Surg 7:879–883
Lin HC, Xirasagar S, Lee HC et al (2006) Hospital volume and inpatient mortality after cancer-related gastrointestinal resections: the experience of an Asian country. Ann Surg Oncol 13:1182–1188
Smith JK, McPhee JT, Hill JS et al (2007) National outcomes after gastric resection for neoplasm. Arch Surg 142:387–393
Learn PA, Bach PB (2010) A decade of mortality reductions in major oncologic surgery: the impact of centralization and quality improvement. Med Care 48:1041–1049
Kim CY, Nam BH, Cho GS et al (2016) Learning curve for gastric cancer surgery based on actual survival. Gastric Cancer 19:631–638
Liang Y, Wu L, Wang X et al (2015) The positive impact of surgeon specialization on survival for gastric cancer patients after surgery with curative intent. Gastric Cancer 18:859–867
Finlayson EV, Goodney PP, Birkmeyer JD (2003) Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg 138:721–725
Dikken JL, Dassen AE, Lemmens VE et al (2012) Effect of hospital volume on postoperative mortality and survival after oesophageal and gastric cancer sur- gery in the Netherlands between 1989 and 2009. Eur J Cancer 48:1004–1013
Lee HH, Son SY, Lee JH et al (2017) Surgeon’s experience overrides the effect of hospital volume for postopera- tive outcomes of laparoscopic surgery in gastric cancer: multi- institutional study. Ann Surg Oncol 24:1010–1017
McCulloch P, Ward J, Tekkis PP, ASCOT Group of Surgeons (2003) British Oesophago-Gastric Cancer Group. Mortality and morbidity in gastro-oesophageal cancer surgery: initial results of ASCOT multicentre prospective cohort study. BMJ 327:1192–1197
Grossmann EM, Longo WE, Virgo KS et al (2002) Morbidity and mortality of gastrectomy for cancer in Department of Veterans Affairs Medical Centers. Surgery 131:484–490
Organization for Economic Cooperation and Development (2011) OECD health data 2011. Organization for Economic Cooperation and Development, Paris
Kim JH, Chin HM, Hwang SS et al (2014) Impact of intra-abdominal fat on surgical outcome and overall survival of patients with gastric cancer. Int J Surg 12:346–352
Wong J, Rahman S, Saeed N et al (2014) Effect of body mass index in patients undergoing resection for gastric cancer: a single center US experience. J Gastrointest Surg 18:505–511
Lee HJ, Kim HH, Kim MC et al (2009) The impact of a high body mass index on laparoscopy assisted gastrectomy for gastric cancer. Surg Endosc 23:2473–2479
Kim HH, Han SU, Kim MC et al (2019) Korean Laparoendoscopic Gastrointestinal Surgery Study (KLASS) Group. Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage I gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol 5:506–513
Nakamura K, Katai H, Mizusawa J et al (2013) A phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric Cancer (JCOG0912). Jpn J Clin Oncol 43:324–327
Etoh T, Japanese Laparoscopic Surgery Study Group (JLSSG). Randomized controlled trial to evaluate laparoscopic versus open surgery for advanced gastric cancer (JLSSG0901: Adv.GC-LAP/OPEN, P II/III). Unique trial number: UMIN000003420 https://upload.umin.ac.jp/cgi-open-bin/ctr/ctr.cgi?function=brows&action=-brows&type = summary&recptno = R000004144&language = E. Accessed 13 Jan 2015
Han SU, Korean Laparoscopic Gastrointestinal Surgery Study (KLASS) Group. Efficacy of laparoscopic subtotal gastrectomy with D2 lymph node dissection for locally advanced gastric cancer (KLASS-02-RCT). ClinicalTrials.gov.http://clinicaltrials.gov/ct2/show/NCT01456598. Accessed 13 Jan 2015
Li G Chinese Laparoscopic Gastrointestinal Surgical Study (CLASS) Group. Multicenter study on laparoscopic distal subtotal gastrectomy for advanced gastric cancer (CLASS-01). Clinical-Trials.gov.http://clinicaltrials.gov/show/NCT01609309. Accessed 13 Jan 2015
Funding
A part of this study was conducted by the financial support from Ministry of Health, Labour and Welfare, Japan (the Health Labour Sciences Research Grant, H30-Seisaku-Shitei-004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest or financial ties to disclose.
Human and animal rights
All procedures were conducted in accordance with the ethical standards of the respective committees on human experimentation (institutional and national) and with the 1964 Declaration of Helsinki and later versions. This study was approved by the Ethics Committee of University of Occupational and Environmental Health, Kitakyushu, Japan.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shibao, K., Fujino, Y., Joden, F. et al. Clinical Outcomes of Laparoscopic Versus Laparotomic Distal Gastrectomy in Gastric Cancer Patients: A Multilevel Analysis Based on a Nationwide Administrative Database in Japan. World J Surg 44, 3852–3861 (2020). https://doi.org/10.1007/s00268-020-05709-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05709-6