Abstract
Background
Pilonidal sinus disease (PSD) is traditionally associated with young male patients. While PSD is rare in Asia and Africa, lifestyles are changing considerably throughout the so-called developed world. We question that PSD is an overwhelmingly male disease and that the proportion of women suffering from PSD is worldwide evenly distributed in a homogenous matter.
Methods
We analysed the world literature published between 1833 and 2018, expanding on the database created by Stauffer et al. Following correction for gender bias with elimination of men-only and women-only studies, data were processed using random-effects meta-analysis in the technique of DerSimonian and Laird.
Results
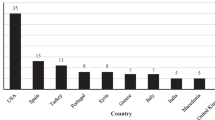
The share of female pilonidal sinus disease patients analysed from all studies available in the world literature is 21%. There are marked regional differences including South America (39%), North America as well as Australia/New Zealand (29%) and Asia (7%), which are highly significant. These results stand fast even if analysis without gender bias corrections was applied.
Conclusion
The share of female patients suffering from PSD is considerable. It is time to think of PSD as a disease of both men and women. Previously unknown, there are significant regional differences worldwide; the reason(s) for the regional differences is still unclear.



Similar content being viewed by others
References
SJEG (2018) Joint statement by the surgery journal editors group. World J Surg 42:2283–2283. https://doi.org/10.1002/jhbp.566
Mansukhani NA, Yoon DY, Teter KA et al (2016) Determining if sex bias exists in human surgical clinical research. JAMA Surg 151:1022–1030
Lundine J, Bourgeault IL, Clark J et al (2019) Gender bias in academia. Lancet 393:741–743
Hayes MM, Fessler HE (2020) Bye-bye gender bias? the promise of a new generation. Ann Am Thorac Soc 17:560–562
Mann S, Ariyanayagam D (2020) Gender bias in medical education: Stop treating it as an inevitability. Med Educ 00:1. https://doi.org/10.1111/medu.14186
Klein R, Julian KA, Snyder ED et al (2019) Gender bias in resident assessment in graduate medical education: review of the literature. J Gen Intern Med 34:712–719
Tam V, Tong B, Gorawara-Bhat R et al (2019) Gender bias affects assessment of frailty and recommendations for surgery. Ann Thorac Surg 109:938–944
Garcia-Gonzalez J, Forcen P, Jimenez-Sanchez M (2019) Men and women differ in their perception of gender bias in research institutions. PLoS ONE 14:e0225763
Nam GB (2018) Gender issues in medical decisions: implicit stereotyping and unconscious bias. Korean Circ J 48:529–531
Mayo H (1833) Observations on injuries and diseases of the rectum. Burgess & Hill, London
Granet E, Ferguson LK (1945) Pilonidal disease. Am J Surg 70:14
Evers T, Doll D, Matevossian E et al (2011) Trends in incidence and long-term recurrence rate of pilonidal sinus disease and analysis of associated influencing factors. Zhonghua Wai Ke Za Zhi 49:799–803
Doll D, Luedi MM, Wieferich K et al (2015) Stop insulting the patient: neither incidence nor recurrence in pilonidal sinus disease is linked to personal hygiene. PSJ 1:11–19
Stauffer VK, Luedi MM, Kauf P et al (2018) Common surgical procedures in pilonidal sinus disease: a meta-analysis, merged data analysis, and comprehensive study on recurrence. Nature 8:3058
Doll D, Orlik A, Maier K et al (2019) Impact of geography and surgical approach on recurrence in global pilonidal sinus disease. Sci Rep 9:15111
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Freeman MF, Tukey JW (1950) Transformations related to the angular and the square root. Ann Math Stat 21:607–611
Vetter TR (2019) Systematic review and meta-analysis: sometimes bigger is indeed better. Anesth Analg 128:575–583
Schober P, Vetter TR (2020) Meta-Analysis in clinical research. Anesth Analg 131:in press
Chijiwa T, Suganuma T, Takigawa T et al (2006) Pilonidal sinus in Japan maritime self-defense force at Yokosuka. Mil Med 171:650–652
Fansler WA, Anderson JK (1934) Case of pilonidal sinus in a negro. Minn Med 17:146
Saleeby E, McCarthy PA (1937) Pilonidal sinus in a negro. Ann Surg 105:634–635
Breidenbach L, Wilson HL (1935) Pilonidal cysts and sinuses. Ann Surg 102:455–463
Tendler MJ, MagGehee JL (1947) Pilonidal sinus (A review of 145 cases). Memphis Med J Memphis 22:192–196
Gips M, Melki Y, Salem L, Weil R, Sulkes J (2008) Minimal surgery for pilonidal disease using trephines: description of a new technique and long-term outcomes in 1,358 patients. DCR 51:1656–1662; discussion 1662–3
Akinci OF, Bozer M, Uzunköy A et al (1999) Incidence and aetiological factors in pilonidal sinus among Turkish soldiers. Eur J Surg 165:339–342
Duman K, Girgin M, Harlak A (2017) Prevalence of sacrococcygeal pilonidal disease in Turkey. Asian J Surg 40:434–437
Alley RL, Richey CO (1945) Pilonidal cyst: excision and primary wound closure. Mil Surg 96:422–423
Sievert H, Evers T, Matevossian E et al (2013) The influence of lifestyle (smoking and body mass index) on wound healing and long-term recurrence rate in 534 primary pilonidal sinus patients. Int J Colorectal Dis 28:1555–1562
Obedman M, Vaticon D (1993) Pilonidal sinus: a high-incidence disease among adolescents. Int J Adolesc Med Health 6:21–36
Duman K, Girgin M, Harlak A (2017) Prevalence of sacrococcygeal pilonidal disease in Turkey. Asian J Surg 40:434–437
Doll D, Krueger CM, Schrank S et al (2007) Timeline of recurrence after primary and secondary pilonidal sinus surgery. DCR 50:1928–1934
Doll D, Friederichs J, Boulesteix AL et al (2008) Surgery for asymptomatic pilonidal sinus disease. Int J Colorectal Dis 23:839–844
Franckowiak JJ, Jackman RJ (1962) The etiology of pilonidal sinus DCR. Dis Colon Rectum 5:28–36
Bosche F, Luedi MM, van der Zypen D et al (2018) The Hair in the sinus: sharp-ended rootless head hair fragments can be found in large amounts in pilonidal sinus nests. World J Surg 42:567–573
Eryilmaz R, Şahin M, Alimoǧlu O et al (2003) Predisposing factors in chronic pilonidal sinus development. Turk J Surg 19:49–53
Schmidt TH, Khanijow K, Cedars MI et al (2016) Cutaneous findings and systemic associations in women with polycystic ovary syndrome. JAMA Dermatol 152:391–398
Kakoly NS, Khomami MB, Joham AE et al (2018) Ethnicity, obesity and the prevalence of impaired glucose tolerance and type 2 diabetes in PCOS: a systematic review and meta-regression. Hum Reprod Update 24:455–467
Lim SS, Kakoly NS, Tan JWJ et al (2019) Metabolic syndrome in polycystic ovary syndrome: a systematic review, meta-analysis and meta-regression. Obes Rev 20:339–352
Parent AS, Teilmann G, Juul A et al (2003) The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev 24:668–693
Doll D, Matevossian E, Wietelmann K et al (2009) Family history of pilonidal sinus predisposes to earlier onset of disease and a 50% long-term recurrence rate. DCR 52:1610–1615
Ardelt M, Dennler U, Fahrner R, Hallof G, Tautenhahn HM, Dondorf F, Rauchfuss F, Settmacher U (2017) [Puberty is a major factor in pilonidal sinus disease : gender-specific investigations of case number development in Germany from 2007 until 2015]. Chirurg 88:961–967
Kallet HI (1936) Pilonidal sinus. The factor of adolescence. Trans Am Proctol Soc 37:203–207
Doll D, Friederichs J, Dettmann H et al (2008) Time and rate of sinus formation in pilonidal sinus disease. Int J Colorectal Dis 23:359–364
Doll D, Bosche FD, Stauffer VK et al (2017) Strength of occipital hair as an explanation for pilonidal sinus disease caused by intruding hair. DCR 60:979–986
Hodges RM (1880) Pilonidal sinus. Boston Med Surg J 103:485–486
Acknowledgements
We acknowledge the editorial assistance of Jeannie Wurz, Science Writer in the Department of Anaesthesiology and Pain Medicine, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland.
Funding
No funding or grants from any other funding agency in the public, commercial or not-for-profit sectors were received. There are no relevant or minor financial relationships between relatives or next of kin and external companies.
Author information
Authors and Affiliations
Contributions
PS, DD, MML and MD performed statistical analysis and calculations. PS, MML, VKS, DD and MD contributed to manuscript editing and interpretation of data. PS, DD, VKS, MML and MD were involved in manuscript writing and critical reviewing. PS, MD, DD and MML designed the graphics. MD and DD performed data acquisition.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Human and animal rights
This article does not contain any studies with human participants, human samples or live vertebrates.
Informed consent
Therefore, informed consent was not required prior to preparation of the current manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luedi, M.M., Schober, P., Stauffer, V.K. et al. Global Gender Differences in Pilonidal Sinus Disease: A Random-Effects Meta-Analysis. World J Surg 44, 3702–3709 (2020). https://doi.org/10.1007/s00268-020-05702-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05702-z