Abstract
Background
The incidences of postoperative pulmonary complications (PPCs) such as atelectasis, pneumonia and pleural effusion after major surgery range from <1 to 23%. Atelectasis after abdominal surgery increases the duration of hospitalization and short-term mortality rate, but there are few reports about atelectasis after hepatectomy. The effectiveness of prone position drainage as physiotherapy has been reported, but it remains unclarified whether prone positioning prevents atelectasis after hepatectomy. This study aimed to evaluate the effect of the prone position on the incidence of atelectasis after hepatectomy.
Methods
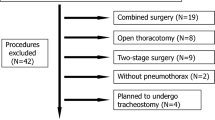
We retrospectively analyzed the incidence of PPCs after hepatectomy at a single center. Patients were divided into two cohorts. The earlier cohort (n = 165) underwent hepatectomy between January 2016 and March 2018 and was analyzed to identify the risk factors for atelectasis and short-term outcomes; the later cohort (n = 51) underwent hepatectomy between April 2018 and March 2019 and underwent prone position drainage in addition to regular mobilization postoperatively. The incidences of PPCs were compared between the two cohorts.
Results
Independent risk factors for atelectasis were anesthetic duration (P = 0.016), operation time (P = 0.046) and open surgery (P = 0.011). The incidence of atelectasis was significantly lower in the later cohort (9.8%) than the earlier cohort (34.5%, P < 0.001). Moreover, the later cohort had a significantly shorter duration of oxygen support (P < 0.001) and postoperative hospitalization (P < 0.001). After propensity score-matching, the incidence of atelectasis remained significantly lower in the later cohort (P = 0.027).
Conclusion
Prone position drainage may decrease the incidence of atelectasis after hepatectomy and improve the short-term outcomes.

Similar content being viewed by others
References
Smetana GW (1999) Preoperative pulmonary evaluation. N Engl J Med 340(12):937–944
Fisher BW, Majumdar SR, McAlister FA (2002) Predicting pulmonary complications after nonthoracic surgery: a systematic review of blinded studies. Am J Med 112(3):219–225
Miskovic A, Lumb AB (2017) Postoperative pulmonary complications. Br J Anesth 118:317–334
Dimick JB, Chen SL, Taheri PA et al (2004) Hospital costs associated with surgical complications; a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 19984:531–537
Lawrence VA, Cornell JE, Smetana GW (2006) Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 144(8):596–608
Merath K, Chen Q, Bagante F et al (2018) Synergistic effects of perioperative complications on 30-day mortality following hepatopancreatic surgery. J Gastrointest Surg 22(10):1715–1723
Wahba RM (1996) Airway closure and intraoperative hypoxaemia: twenty-five years later. Can J Anesth 43(11):1144–1149
Rosenberg J, Ullstad T, Rasmussen J et al (1994) Time course of postoperative hypoxaemia. Eur J Surg 160(3):137–143
Powell JF, Menon DK, Jones JG (1996) The effects of hypoxaemia and recommendations for postoperative oxygen therapy. Anesthesia 51(8):769–772
Rothen HU, Sporre B, Engberq G et al (1995) Prevention of atelectasis during general anesthesia. Lancet 345:1387–1391
van Kaan AH, Lachmann RA, Herting E et al (2004) Reducing atelectasis attenuates bacterial growth and translocation in experimental pneumonia. Am J Respir Crit Care Med 169(9):1046–1053
Kallet RH (2015) A comprehensive review of prone position in ARDS. Respir Care 60(11):1660–1687
Pelosi P, Caironi P, Taccone P et al (2001) Pathophysiology of prone positioning in the healthy lung and in ALI/ARDS. Minerva Anestesiol 67(4):238–247
De Jong A, Molinari N, Sebbane M et al (2013) Feasibility and effectiveness of prone position in morbidly obese patients with ARDS. Chest 143(6):1554–1561
Koch M, Garden OJ, Padbury R et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149(5):680–688
Rahbari NN, Garden OJ, Padbury R et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery. Surgery 149(5):713–724
Brooks-Brunn JA (1995) Postoperative atelectasis and pneumonia: risk factors. Am J clit Care 4(5):340–349
Smith PR, Baig MA, Brito V et al (2010) Postoperative pulmonary complications after laparotomy. Respiration 80(4):269–274
Khuri SF, Henderson WG, DePalma RG et al (2005) Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 242(3):326–343
Foster CA, Charles EJ, Turrentine FE et al (2019) Development and validation of procedure-specific risk score for predicting postoperative pulmonary complication: a NSQIP analysis. J Am Coll Surg 229(4):355–365
Mazo V, Sabate S, Canet J et al (2014) Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology 121(2):219–231
Yang CK, Teng A, Lee DY et al (2015) Pulmonary complications after major abdominal surgery: national surgical quality improvement program analysis. J Surg Res 198(2):441–449
Hua M, Brady JE, Li G (2012) A scoring system to predict unplanned intubation in patients having undergone major surgical procedures. Anesth Analg 115(2):88–94
McAlister FA, Bertsch K, Man J et al (2005) Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med 171(5):514–517
Abroug F, Ouanes-Besbes L, Elatrous S et al (2008) The effect of prone positioning in acute respiratory distress syndrome or acute lung injury: a meta-analysis. Areas of uncertainty and recommendations for research. Intensive Care Med 34(6):1002–1011
Pelosi P, Croci M, Calappi E et al (1996) Prone positioning improves pulmonary function in obese patients during general anesthesia. Anesth Analg 83(3):578–583
Acknowledgements
We thank Kelly Zammit, BVSc, from Edanz Group (https://en-author-services.edanzgroup.com/) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Toshida, K., Minagawa, R., Kayashima, H. et al. The Effect of Prone Positioning as Postoperative Physiotherapy to Prevent Atelectasis After Hepatectomy. World J Surg 44, 3893–3900 (2020). https://doi.org/10.1007/s00268-020-05682-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05682-0