Abstract
Background
Non-occlusive mesenteric ischemia (NOMI) has a high mortality rate, but the analyses of preoperative prognostic factors for improving survival in patients suspected of having NOMI are scarce. We aimed to analyze the prognostic factors of preoperative examinations for NOMI.
Methods
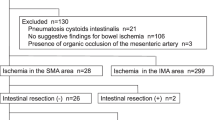
The clinical data of 224 patients with NOMI were retrospectively collected for a multicenter survey. Clinicophysiological factors were compared between the survivors and non-survivors (N = 107/117) and between the operative and non-operative cases (N = 180/44) by univariate analysis using chi-square test and multivariate analysis using Cox proportional hazard models. In the operative cases, the prognostic operative factors were also analyzed.
Results
The overall mortality rate for NOMI was 52.2%. There were 129 male and 95 female patients. The mean age was 71.23 (14–94) years. Univariate analysis showed that cardiovascular complication, shock, abdominal pain, average blood pressure, systemic inflammatory response syndrome, aspartic aminotransferase, alanine transaminase, creatine phosphokinase, lactate dehydrogenase, base excess, prothrombin time-international normalized ratio, D-dimer, and fibrinogen degradation products were independent prognostic factors. Multivariate analysis showed that average blood pressure and base excess were independent prognostic factors. Among patients undergoing surgery, those with bowel resection had better prognosis than those without bowel resection, but those with long bowel resection had worse prognosis than those with short resection. Additional postoperative treatment was not effective compared with operation alone (P = 0.011).
Conclusions
Prognostic factors of preoperative examinations for NOMI were average blood pressure and base excess. Patients with long bowel resection should be carefully monitored owing to their poor prognosis.
Similar content being viewed by others
References
Ende N (1958) Infarction of the bowel in cardiac failure. N Engl J Med 258:879–881
Woodhams R, Nishimaki H, Fujii K et al (2010) Usefulness of multidetector-row CT (MDCT) for the diagnosis of non-occlusive mesenteric ischemia (NOMI): assessment of morphology and diameter of the superior mesenteric artery (SMA) on multi-planar reconstructed (MPR) images. Eur J Radiol 76:96–102
Britt LG, Cheek RC (1969) Nonocclusive mesenteric vascular disease: clinical and experimental observations. Ann Surg 169:704–711
Howard TJ, Plaskon LA, Wiebke EA et al (1996) Nonocclusive mesenteric ischemia remains a diagnostic dilemma. Am J Surg 171:405–408
Klotz S, Vestring T, Rötker J et al (2001) Diagnosis and treatment of nonocclusive mesenteric ischemia after open heart surgery. Ann Thorac Surg 72:1583–1586
Trompeter M, Brazda T, Remy CT et al (2002) Non-occlusive mesenteric ischemia: etiology, diagnosis, and interventional therapy. Eur Radiol 12:1179–1187
John AS, Tuerff SD, Kerstein MD (2000) Nonocclusive mesenteric infarction in hemodialysis patients. J Am Coll Surg 190:84–88
Mitsuyoshi A, Obama K, Shinkura N et al (2007) Survival in nonocclusive mesenteric ischemia: early diagnosis by multidetector row computed tomography and early treatment with continuous intravenous high-dose prostaglandin E(1). Ann Surg 246:229–235
Lock G (2001) Acute intestinal ischaemia. Best Pract Res Clin Gastroenterol 15:83–98
Groesdonk HV, Klingele M, Schlempp S et al (2013) Risk factors for nonocclusive mesenteric ischemia after elective cardiac surgery. J Thorac Cardiovasc Surg 145:1603–1610
Bone RC, Balk RA, Cerra FB et al (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Prager M, Teufelsbauer H, Nanobashvili J et al (2000) Abdominal vascular surgery emergencies: abdominal aortic aneurysm, acute mesenteric ischemia—indications, technique, results. Acta Med Austriaca 27:145–151
Pérez-García C, de Miguel CE, Fernández Gonzalo A et al (2018) Non-occlusive mesenteric ischaemia: CT findings, clinical outcomes and assessment of the diameter of the superior mesenteric artery. Br J Radiol 91:20170492
Siegelman SS, Sprayregen S, Boley SJ (1974) Angiographic diagnosis of mesenteric arterial vasoconstriction. Radiology 112:533–542
Nakamura Y, Urashima M, Toyota N et al (2013) Non-occlusive mesenteric ischemia (NOMI): utility of measuring the diameters of the superior mesenteric artery and superior mesenteric vein at multidetector CT. Jpn J Radiol 31:737–743
Stroeder J, Klingele M, Bomberg H et al (2017) Occurrence and severity of non-occlusive mesenteric ischemia (NOMI) after cardiovascular surgery correlate with preoperatively assessed FGF-23 levels. PLoS ONE 12:e0182670
Daviaud F, Grimaldi D, Dechartres A et al (2015) Timing and causes of death in septic shock. Ann Intensive Care 5:16
Guillaume A, Pili-Floury S, Chocron S et al (2017) Acute mesenteric ischemia among postcardiac surgery patients presenting with multiple organ failure. Shock 47:296–302
Stockmann H, Roblick UJ, Kluge N et al (2000) Diagnosis and therapy of non-occlusive mesenteric ischemia (NOMI). Zentralbl Chir 125:144–151
Quiroga B, Verde E, Abad S et al (2013) Detection of patients at high risk for non-occlusive mesenteric ischemia in hemodialysis. J Surg Res 180:51–55
Yukaya T, Saeki H, Taketani K et al (2014) Clinical outcomes and prognostic factors after surgery for non-occlusive mesenteric ischemia: a multicenter study. J Gastrointest Surg 18:1642–1647
Pessina AC, Palatini P, Sperti G et al (1985) Evaluation of hypertension and related target organ damage by average day-time blood pressure. Clin Exp Hypertens A 7:267–278
Vollmar B, Menger MD (2011) Intestinal ischemia/reperfusion: microcirculatory pathology and functional consequences. Langenbecks Arch Surg 396:13–29
Kvarstein G, Mirtaheri P, Tønnessen TI (2003) Detection of organ ischemia during hemorrhagic shock. Acta Anaesthesiol Scand 47:675–686
Reginelli A, Lacobellis F, Berritto D et al (2013) Mesenteric ischemia: the importance of differential diagnosis for the surgeon. BMC Surg 13(Suppl2):S51
Acosta-Merida MA, Marchena-Gomez J, Hemmersbach-Miller M et al (2006) Identification of risk factors for perioperative mortality in acute mesenteric ischemia. World J Surg 30:1579–1585
Ward D, Vernava AM, Kaminski DL et al (1995) Improved outcome by identification of high-risk nonocclusive mesenteric ischemia, aggressive reexploration, and delayed anastomosis. Am J Surg 170:577–580
Irie T, Matsutani T, Hagiwara N et al (2017) Successful treatment of non-occlusive mesenteric ischemia with indocyanine green fluorescence and open-abdomen management. Clin J Gastroenterol 10:514–551
Nakamura F, Yui R, Muratsu A et al (2019) Study of the prognostic factor of the colon perforation case with the pan-peritonitis that needed emergency surgery: a single-center observational study. Acute Med Surg 6:379–384
Acknowledgments
This study was a nationwide multi-institutional analysis of NOMI conducted by the board members of the Japanese Society for Abdominal Emergency Medicine. The authors thank the following participating institutions: Medical Emergency Center Kinki University, Yashima General Hospital, Ebina General Hospital, Department of Gastroenterological Surgery Hirosaki University, Department of Surgery Nippon Medical School Chiba Hokusoh Hospital, Hyogo Prefectural Awaji Medical Center, Department of Gastroenterological Surgery II, Hokkaido University, National Hospital Organization Chiba Medical Center, Department of Gastroenterology Toho University Ohashi Medical Hospital, Advanced Emergency Medical Service Center Kurume University, Department of General and Mammary Endocrine Surgery Sapporo Medical University, Public Toyooka Hospital, Trauma and Resuscitation Saga University, Department of Inflammatory Bowel Disease, Division of Surgery Hyogo College of Medicine, First Department of Surgery Dokkyo Medical University, Department of Surgery and Science, Graduate School of Medical Sciences Kyushu University, Department of Surgery Showa General Hospital, Department of Colorectal and Proctological Surgery Juntendo University, Department of Surgery Jikei University, Advanced Critical Care Center, Radiology Department Gifu University, Department of Gastrointestinal Surgery, Saitama Medical University, First Department of Surgery Yamagata University, Emergency General Center Higashisumiyoshi Morimoto Hospital, Department of Digestive and General Surgery St. Marianna University School of Medicine, General Medical Treatment/Emergency Center Toho University Omori Medical Center, Division of Emergency and Critical Care Medicine Tohoku University Graduate School of Medicine.
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical conduct
This study was approved by the research Ethics Committee of Ibaraki Medical Center, Tokyo Medical University (acceptance number: 15–9) and the research Ethics Committee of Japanese Society for Abdominal Emergency Medicine. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration. This article does not contain any studies with animals performed by any of the authors.
Informed consent
The requirement for obtaining written informed consent from each patient was waived because of the retrospective study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suzuki, S., Kondo, H., Furukawa, A. et al. Prognostic Factors of Preoperative Examinations for Non-occlusive Mesenteric Ischemia: A Multicenter Retrospective Project Study Conducted by the Japanese Society for Abdominal Emergency Medicine. World J Surg 44, 3687–3694 (2020). https://doi.org/10.1007/s00268-020-05678-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05678-w